Summary of Notifiable Infectious Diseases and Conditions — United States, 2015
Weekly / August 11, 2017 / 64(53);1–143
Deborah A. Adams1; Kimberly R. Thomas, MPH1; Ruth Ann Jajosky, DMD1; Loretta Foster, MPH1; Gitangali Baroi, MPH1; Pearl Sharp1; Diana H. Onweh1; Alan W. Schley1; Willie J. Anderson1; for the Nationally Notifiable Infectious Conditions Group (View author affiliations)
View suggested citation- pdf icon [PDF]
Preface
The Summary of Notifiable Infectious Diseases and Conditions — United States, 2015 (hereafter referred to as the summary) contains the official statistics, in tabular and graphical form, for the reported occurrence of nationally notifiable infectious diseases and conditions in the United States for 2015. Unless otherwise noted, data are final totals for 2015 reported as of June 30, 2016. These statistics are collected and compiled from reports sent by U.S. state and territories, New York City, and District of Columbia health departments to the National Notifiable Diseases Surveillance System (NNDSS), which is operated by CDC in collaboration with the Council of State and Territorial Epidemiologists (CSTE). This summary is available at https://www.cdc.gov/MMWR/MMWR_nd/index.html. This site also includes summary publications from previous years.
The Highlights section presents noteworthy epidemiologic and prevention information for 2015 for selected infectious diseases and conditions and additional information to aid in the interpretation of surveillance and infectious diseases and conditions-trend data. Part 1 contains tables showing incident (new) cases and incidence rates for the nationally notifiable infectious diseases and conditions reported during 2015; these tables do not include rows for conditions with zero cases reported in 2015 (Tables 1, 2, 3, 4, 5, 6, and 7).* The tables provide the number of cases reported to CDC for 2015 and the distribution of cases by geographic location, MMWR month (MMWR month is based upon MMWR year and week, which is described in the Interpreting Data section of this report), and demographic characteristics (e.g., age, sex, race, and ethnicity). Table 1 is new to the summary and displays the national incidence count and rate for each nationally notifiable disease and condition. Tables 2 and 3 reflect content format from previous summaries. Tables 4–7, which have been an integral component of the summary for decades, also include incidence rates. Part 2 contains graphs and maps that depict summary data for selected notifiable infectious diseases and conditions described in tabular form in Part 1. The following tables in previous releases are no longer included in the summary: a table with the historical reported incidence of notifiable diseases and conditions and a table enumerating deaths associated with specified notifiable infectious diseases and conditions reported to CDC’s National Center for Health Statistics (NCHS), which were previously included in Part 3 of the summary. Historical notifiable disease data during 1944–2014 are available online in previous years’ summaries (https://www.cdc.gov/MMWR/MMWR_nd). The Selected Reading section presents general and disease-specific references for notifiable infectious diseases and conditions. These references provide additional information on surveillance and epidemiologic concerns, diagnostic concerns, and infectious disease-control activities.
Background
The infectious diseases and conditions designated by CSTE and CDC as nationally notifiable during 2015 are listed in this section. A notifiable infectious disease or condition is one for which regular, frequent, and timely information regarding individual cases is considered necessary for the prevention and control of the disease or condition. A brief history of the reporting of nationally notifiable infectious diseases and conditions in the United States is available at https://wwwn.cdc.gov/nndss/history.aspx. In 1961, CDC assumed responsibility for the collection of data on nationally notifiable diseases. Data are collected through NNDSS, which is neither a single surveillance system nor a method of reporting. Rather, it is a “system of systems,” which is coordinated by CDC at the national level across disease-specific programs to optimize data compilation, analysis, and dissemination of notifiable disease data. Monitoring surveillance data enables public health authorities to detect sudden changes in disease or condition occurrence and distribution, identify changes in agents and host factors, and detect changes in health care practices. National-level surveillance data are compiled from case notification reports of nationally notifiable infectious diseases and conditions submitted from the state, territory, and selected local health departments to CDC.
Cases are first identified through reports of infectious diseases and conditions from the local level to the state or territory. Legislation, regulation, or other rules in those jurisdictions require health care providers, hospitals, laboratories, and others to provide information on reportable conditions to public health authorities or their agents. Case reporting at the local level protects the public’s health by ensuring the proper identification and follow-up of cases. Public health workers ensure that persons who are already ill receive appropriate treatment; trace contacts who need vaccines, treatment, quarantine, or education; investigate and control outbreaks; eliminate environmental hazards; and close premises where disease transmission is believed to be ongoing.
Although infectious disease and condition reporting is mandated at the state, territory, and local levels by legislation or regulation, state and territory notification to CDC is voluntary. All U.S. state health departments, five territorial health departments, and two local health departments (New York City and District of Columbia) voluntarily notify CDC about nationally notifiable infectious diseases and conditions that are reportable in their jurisdictions; the data in the case notifications that CDC receives are collected by staff working on reportable disease and condition surveillance systems in local, state, and territorial health departments. Case notification of nationally notifiable infectious diseases and conditions helps public health authorities monitor the effect of these diseases and conditions, measure the disease and condition trends, assess the effectiveness of control and prevention measures, identify populations or geographic areas at high risk, allocate resources appropriately, formulate prevention strategies, and develop public health policies.
The list of nationally notifiable infectious diseases and conditions is revised periodically (Box 1). An infectious disease or condition might be added to the list as a new pathogen emerges, or a disease or condition might be removed as its incidence declines. Public health officials at state and territorial health departments collaborate with CDC staff in determining which infectious diseases and conditions should be considered nationally notifiable. CSTE, with input from CDC, makes recommendations annually for additions and deletions to the list. The list of infectious diseases and conditions considered reportable in each jurisdiction varies over time and across jurisdictions. Current and historical national public health surveillance case definitions used for classifying and enumerating cases consistently at the national level across reporting jurisdictions are available at https://wwwn.cdc.gov/nndss/conditions.
Data Sources
Provisional data on the reported occurrence of nationally notifiable infectious diseases and conditions are published weekly in MMWR. After each reporting year, staff in state and territorial health departments finalize reports of cases for that year with local or county health departments and reconcile the data with reports previously sent to CDC throughout the year.
These data are compiled in final form in this summary, which represents the official and archival counts of cases for each year. The data in these reports are approved by the appropriate chief epidemiologist from each submitting state or territory before being published in this summary. Data published in MMWR Surveillance Summaries or other surveillance reports produced by CDC programs might differ from data reported in this summary because of differences in the timing of reports, the source of the data, or surveillance methodology.
Data in this summary were derived primarily from reports transmitted to CDC from health departments in the 50 states, five territories, New York City, and the District of Columbia (reporting jurisdictions). Data were reported for MMWR weeks 1–52, which correspond to the period for the week ending January 10, 2015 through the week ending January 2, 2016. Information about how MMWR weeks are defined by jurisdictions is presented in the Interpreting Data section of this report. More information regarding notifiable infectious diseases and conditions, including national surveillance case definitions, is available at https://wwwn.cdc.gov/nndss/conditions. Policies for reporting notifiable infectious disease and condition cases can vary by disease, condition, or reporting jurisdiction. The case-status categories used to determine which cases reported to NNDSS are published in the tables are listed by infectious disease or condition in the publication criteria column of the 2015 NNDSS event code list (Box 2).
For a report of a nationally notifiable disease or condition to be published in MMWR (formerly described as “print criteria” and currently described as “publication criteria”), the reporting state or territory must have designated the infectious disease or condition reportable in their state or territory for the year corresponding to the year of report to CDC. After this criterion is met, the infectious disease- or condition-specific criteria listed in Box 2 are applied. When “all reports” is listed for the publication criteria, this means that cases designated with unknown or suspect case confirmation status will be included in the counts along with probable and confirmed cases. Data for new nationally notifiable infectious diseases or conditions are not usually available from reporting jurisdictions until January of the year following the approval of the CSTE position statement. In addition, CDC must have Office of Management and Budget Paperwork Reduction Act approval to request data from reporting jurisdictions (1). As a result, there is usually a delay between the time that CSTE recommends a condition be made nationally notifiable and the time CDC can aggregate the data submitted by reporting jurisdictions.
Final data for certain infectious diseases and conditions are derived from the surveillance records of the CDC program. Requests for further information regarding these data should be directed to the appropriate program. The CDC programs responsible for finalizing the data used for the final MMWR tables for each condition are listed (Box 2).
Population estimates were obtained from the NCHS postcensal estimates of the resident population of the United States during July 1, 2015–July 1, 2016, by year, county, single year of age (range: 0 to ≥85 years), bridged-race (white, black or African American, American Indian or Alaska Native, Asian, or Pacific Islander), Hispanic ethnicity (not Hispanic or Latino, Hispanic or Latino), and sex (Vintage 2015), prepared under a collaborative arrangement with the U.S. Census Bureau. Population estimates for states as of June 28, 2016 are available at https://www.cdc.gov/nchs/nvss/bridged_race/data_documentation.htm. Population estimates for territories are from the 2015 U.S. Census Bureau International Data Base and are available at https://www.census.gov/population/international/data/idb/informationGateway.phpexternal icon. The choice of population denominators for incidence reported in MMWR is based on the availability of census population data at the time of publication preparation and the desire for consistent use of the same population data to compute incidence reported by different CDC programs.
Incidence in this summary was calculated as the number of reported cases for each infectious disease or condition divided by either the U.S. resident population for the specified demographic population or the total U.S. resident population, multiplied by 100,000. For territories, incidence in this summary was calculated as the number of reported cases for each infectious disease or condition divided by either the territorial resident population for the specified demographic population or the total territorial resident population, multiplied by 100,000. When a nationally notifiable infectious disease or condition was associated with a specific restriction (e.g., age, sex, race, or ethnicity), the same restriction was applied to the population in the denominator of the incidence calculation. In addition, population data from states in which the disease or condition was not reportable or was not available are excluded from incidence calculations. Unless otherwise stated, disease totals for the United States do not include data for American Samoa, Guam, Puerto Rico, the Commonwealth of the Northern Mariana Islands, or the U.S. Virgin Islands.
Interpreting Data
The completeness of information on notifiable infectious diseases and conditions was highly variable and related to the disease or condition being reported (2–9). Incidence data in this summary are presented by the MMWR week and year (https://wwwn.cdc.gov/nndss/document/MMWR_Week_overview.pdfpdf icon) assigned by the state or territorial health department, with some exceptions, including human immunodeficiency virus (HIV) (presented by date of diagnosis), tuberculosis (presented by date that the reporting jurisdiction verified that the case met the criteria in the national surveillance case definition), domestic arboviral diseases (presented by date of illness onset), and varicella deaths (presented by date of death). The calendar days corresponding to MMWR weeks for MMWR year 2015 are available at https://wwwn.cdc.gov/nndss/document/w2014-15.pdfpdf icon. MMWR month is derived from MMWR weeks. Data were reported by the jurisdiction of the person’s “usual residence” at the time of disease or condition onset (https://wwwn.cdc.gov/nndss/document/11-SI-04.pdfpdf icon). For certain nationally notifiable infectious diseases and conditions, surveillance data are reported independently to various CDC programs. For this reason, surveillance data reported by other CDC programs might vary from data reported in this summary because of differences in 1) the date used to aggregate data (e.g., date of report or date of disease or condition occurrence), 2) the timing of reports, 3) the source of the data, 4) surveillance case definitions, and 5) policies regarding case jurisdiction (i.e., which jurisdiction should submit the case notification to CDC). In addition, the “date of disease occurrence” of conditions might vary. For infectious diseases, the meaning of the “date of disease occurrence” varies across jurisdictions and by disease and might be a date of symptom or disease onset, diagnosis, laboratory result, reporting of a case to a jurisdiction, or notification of a case to CDC.
Data reported in this summary are useful for analyzing infectious disease or condition trends and determining relative infectious disease or condition numbers. However, reporting practices affect how these data should be interpreted. Infectious disease and condition reporting is likely incomplete, and completeness might vary depending on the infectious disease or condition and reporting state. The degree of completeness of data reporting also might be influenced by the diagnostic facilities available, control measures in effect, public awareness of a specific infectious disease or condition, and the resources and priorities of state and local officials responsible for public health surveillance and for controlling infectious diseases and conditions. Finally, factors such as changes in methods for public health surveillance, introduction of new diagnostic tests, or discovery of new infectious disease or condition entities can cause changes in reporting that are independent of the actual incidence of infectious disease or condition.
Public health surveillance data are published for selected racial and ethnic populations because these characteristics can be risk markers for certain notifiable infectious diseases or conditions. Race and ethnicity data also can be used to highlight populations for focused prevention programs. However, caution must be used when drawing conclusions from reported race and ethnicity. Different racial and ethnic populations might have different patterns of access to health care, potentially resulting in data that are not representative of actual infectious disease or condition incidence among specific population groups. In addition, not all race and ethnicity data are collected or reported uniformly for all infectious diseases and conditions; for example, the recommended standard for classifying a person’s race or ethnicity is based on self-report. However, this procedure might not always be followed.
Surveillance data reported to NNDSS are in either individual case-specific form or summary form (i.e., aggregated data for a group of cases). Summary data often lack demographic information (e.g., race); therefore, the demographic-specific rates presented in this summary might be underestimated.
Transitions in NNDSS Data Collection
Data collection in NNDSS has undergone various transitions over time. Before 1990, data were reported to CDC as cumulative counts rather than as individual case reports. In 1990, using the National Electronic Telecommunications System for Surveillance (or NETSS), states began electronically capturing and reporting individual cases to CDC without personal identifiers. In 2001, CDC launched the National Electronic Disease Surveillance System (NEDSS) to promote the use of data and information system standards that advance the development of efficient, integrated, and interoperable surveillance information systems at the local, state, territorial, and national levels. Reporting jurisdictions now use integrated surveillance information systems based on NEDSS architectural standards to submit NNDSS data to CDC. Additional information concerning NEDSS is available at https://wwwn.cdc.gov/nndss/nedss.aspx.
In 2013, CDC began to conceptualize improvements to strengthen and modernize the technical infrastructure supporting NNDSS. In 2014, CDC and selected states began work on the NNDSS Modernization Initiative (NMI), a multiyear commitment to enhance NNDSS surveillance capabilities. An important benefit for public health decision making will be the ability to acquire higher quality data that are more comprehensive and timely. Through NMI, CDC and its state partners will increase the robustness of the NNDSS technological infrastructure so that it is based on interoperable, standardized data and data exchange mechanisms. Additional information is available at https://www.cdc.gov/nmi.
Method for Identifying Which Nationally Notifiable Infectious Diseases and Conditions are Reportable
Reportable conditions are determined by the laws and regulations of each state, territory, or local jurisdiction. Some infectious diseases and conditions deemed nationally notifiable by CSTE might not be designated as reportable in certain states or jurisdictions. Only data from reporting states, territories, and jurisdictions that designated the infectious disease or condition as reportable are included in the summary tables. This ensures that the data displayed in this summary are from population-based surveillance efforts and are generally comparable across states, territories, and other jurisdictions. When a CSTE- and CDC-recommended nationally notifiable disease or condition is not reportable by state, territory, or other jurisdiction, an “N” indicator for “not reportable” is inserted in the table or map for the specified reporting state, territory, or jurisdiction and applicable year. Each year, the NNDSS Data Processing Team solicits information from each NNDSS reporting state, territory, and jurisdiction (all 50 U.S. states, the District of Columbia, New York City, and five U.S. territories) about whether reporting is mandated by law or regulation for each nationally notifiable condition.
International Health Regulations
At its annual meeting in June 2007, CSTE approved a position statement that supports implementation of International Health Regulations (IHR) in the United States (10). CSTE approval followed the adoption of revised IHR in May 2005 by the World Health Assembly (11) that went into effect in the United States on July 18, 2007. This international legal instrument governs the role of the World Health Organization (WHO) and its member countries, including the United States, in identifying, responding to, and sharing information about events that might constitute a Public Health Emergency of International Concern (PHEIC). A PHEIC is an extraordinary event that constitutes a public health risk to other countries through international spread of disease and potentially requires a coordinated international response. All WHO member countries are required to notify WHO of a potential PHEIC. WHO makes the final determination about the existence of a PHEIC.
Health care providers in the United States are required to report diseases, conditions, and outbreaks determined to be reportable by local, state, or territorial law or regulation. In addition, all health care providers should work with their local, state, or territorial health agencies to identify and report events occurring in their location that might constitute a PHEIC. U.S. state and territorial departments of health report information about a potential PHEIC to the most relevant federal agency responsible for monitoring such an event. In the case of human diseases, the U.S. state or territorial departments of health notifies CDC through existing formal and informal reporting mechanisms (10). CDC further analyzes the event by use of the decision algorithm in Annex 2 of the IHR and notifies the U.S. Department of Health and Human Services (DHHS) Secretary’s Operations Center (SOC), as appropriate. The DHHS SOC is responsible for reporting a potential PHEIC to WHO.
In the United States, DHHS has the lead role in carrying out IHR, in cooperation with multiple federal departments and agencies. When a potential PHEIC is identified, the United States has 48 hours to assess the risk for the reported event. If authorities determine that a potential PHEIC exists, the United States, as with all WHO member countries, has 24 hours to report the event to WHO.
An IHR decision algorithm (Annex 2 of the IHR) was developed to help countries determine whether an event should be reported. If any two of the following four questions are answered in the affirmative, then a potential PHEIC exists and WHO should be notified:
-
Is the public health impact of the event serious?
-
Is the event unusual or unexpected?
-
Is there a significant risk for international spread?
-
Is there a significant risk for international travel or trade restrictions?
The revised IHR reflects a conceptual shift from the use of a predefined disease list to a framework of reporting and responding to events on the basis of an assessment of public health criteria, including seriousness, unexpectedness, and international travel and trade implications. A PHEIC is an event that falls within those criteria (further defined in a decision algorithm in Annex 2 of the revised IHR); however, any one of the following four conditions always constitutes a PHEIC and do not require the use of the IHR decision instrument in Annex 2:
-
severe acute respiratory syndrome (SARS),
-
smallpox,
-
poliomyelitis caused by wild-type poliovirus, and
-
human influenza caused by a new subtype.
Examples of events that require the use of the decision instrument include, but are not limited, to cholera, pneumonic plague, yellow fever, West Nile fever, viral hemorrhagic fevers, and meningococcal disease. Other biologic, chemical, or radiologic events that fit the decision algorithm also must be reported to WHO.
Additional information about IHR is available at https://www.who.int/ihr/publications/9789241580496/enexternal icon, https://www.cdc.gov/globalhealth/ihregulations.htm, and https://www.cdc.gov/globalhealth/healthprotection/ghs/ihr/index.html. CSTE also approved a position statement that added initial detections of novel influenza A virus infections to the list of nationally notifiable infectious diseases, beginning in January 2007 to, in part, support the implementation of the revised IHR in the United States to identify human influenza caused by a new subtype (12).
Future Plans for Publication of Data on Notifiable Infectious Diseases and Conditions
To improve the usability, availability, quality, and timeliness of surveillance data (13), as part of the CDC Surveillance Strategy, CDC will provide users a convenient way to access notifiable infectious disease data through the National NNDSS website beginning in November 2017.
CDC has redesigned the data and statistics section of the NNDSS website to be a one-stop-shop for users to find both detailed information about the notifiable infectious disease data and the data tables themselves. Although these data will no longer be published in their current format as the MMWR Summary of Notifiable Infectious Diseases and Conditions, users may easily access the information on the NNDSS website. To ease the transition, MMWR also will link users from its website to the new location on the NNDSS website.
Beginning with 2016 data, expected to be published in November 2017, the introductory information in the front of the MMWR Summary report (from the Preface to the Revised International Health Regulations) will be available on the NNDSS Data and Statistics page at https://wwwn.cdc.gov/nndss/data-and-statistics.html. In addition, the redesigned page will provide links to Tables 1–7 available in HTML, text, and PDF formats and hosted on the CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) platform.
Consolidating the notifiable infectious disease data on the NNDSS website is part of the NNDSS Modernization Initiative (NMI) strategy to streamline NNDSS and access to data for users; NMI is a component of the CDC Surveillance Strategy. This consolidation of information also is in response to the recommendations of a CDC-wide workgroup comprising representatives from the CDC Excellence in Science Committee, the Surveillance Science Advisory Group, and MMWR for CDC to make more data available online and to allow MMWR to focus on publishing scientific and actionable surveillance reports and not routine data tables.
Acknowledgments
We acknowledge all the local, state, and territorial health departments in the United States for collecting the data included in this report from a range of case ascertainment sources (e.g., health care providers, hospitals, and laboratories) and for reporting these data to CDC.
Nationally Notifiable Infectious Conditions Group
Elizabeth Adam, MPH; Aileen Artus, MPH; Kelly Barrett, MPH; Albert E. Barskey, MPH; Kaitlin Benedict, MPH; David D. Blaney, MD; Jesse Blanton, MPH; William A. Bower, MD; Jim Braxton; Elizabeth C. Briere, MD; Erin K. Burdette, MPH; Shannon Casillas, MPH; Kevin Chatham-Stephens, MD; Cara Cherry, DVM; Tom M. Chiller, MD; Nakia Clemmons, MPH; Amanda Conrad, MPH; Kasey E. Diebold, MS; Naomi Drexler, MPH; Seth Edmunds, MPH; Amanda E. Faulkner, MPH; Marc Fisher, MD; Kathleen E. Fullerton, MPH; Paul Gastañaduy, MD; Elizabeth B. Gray, MPH; Rebecca Hall, MPH; Alesia Harvey; Katherine A. Hendricks, MD; Barbara L. Herwaldt, MD; Alex R. Hoffmaster, PhD; Michael J. Hughes, MPH; Jennifer C. Hunter, DrPH; Jacqueline Hurd, MPH; Michele Hvlasa, MPH; Shareen A. Iqbal, PhD; Brendan R. Jackson, MD; Jeffrey Jones, MD; Michael C. Judd, MPH; Matt Karwowski, MD; Grishma Kharod, MPH; Kristen Kreisel, PhD; Kiersten J. Kugeler, PhD; Adam J. Langer, DVM; Adia Lee, MSPH; Jennifer Lehman; Nicole Lindsey, MS; Lindy Liu, MPH; Adriana S. Lopez, MHS; Jessica R. MacNeil, MPH; Lilia P. Manangan, MPH; Mona Marin, MD; Orion McCotter, MPH; Daeshonna McNealy, MPH; Paul S. Mead, MD; Maria Negron, DVM; Kristen Nichols Heitman, MPH; Manisha Patel, MD; Emily G. Pieracci, DVM; Robert H. Pratt; Rodney Presley, PhD; Susan Redd; Janell Routh, MD; Anna Satcher Johnson, MPH; Ilana J. Schafer, DVM; Amy M. Schwartz, MPH; Tyler M. Sharp, PhD; Tami H. Skoff, MS; Erin Staples, MD; Tejpratap S. P. Tiwari, MD; Elizabeth Torrone, PhD; Rita M. Traxler, MHS; Antonio R. Vieira, DVM; Ryan M. Wallace, DVM; Karen K. Wong, MD; Jonathan S. Yoder, MPH, CDC.
* No cases of anthrax; Crimean-Congo hemorrhagic fever; dengue hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola hemorrhagic fever; Guanarito hemorrhagic fever; Junin hemorrhagic fever; Lujo virus; Machupo hemorrhagic fever; Marburg fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia-associated hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease (SARS-CoV); smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
References
- US Department of Health and Human Services. Information Collection and Paperwork Reduction Act (PRA) overview. Washington, DC: US Department of Health and Human Services; 2015. https://www.usability.gov/how-to-and-tools/guidance/pra-overview.htmlexternal icon
- Doyle TJ, Glynn MK, Groseclose SL. Completeness of notifiable infectious disease reporting in the United States: an analytical literature review. Am J Epidemiol 2002;155:866–74. CrossRefexternal icon PubMedexternal icon
- CDC. Assessing completeness of perinatal hepatitis B virus infection reporting through comparison of immunization program and surveillance data—United States. MMWR Morb Mortal Wkly Rep 2011;60:410–3. PubMedexternal icon
- CDC. Evaluation of acute hepatitis C infection surveillance—United States, 2008. MMWR Morb Mortal Wkly Rep 2010;59:1407–10. PubMedexternal icon
- Hwang J, McClintock S, Kachur SP, Slutsker L, Arguin P. Comparison of national malaria surveillance system with the national notifiable diseases surveillance system in the United States. J Public Health Manag Pract 2009;15:345–51. CrossRefexternal icon PubMedexternal icon
- Painter JE, Hlavsa MC, Collier SA, Xiao L, Yoder JS. Cryptosporidiosis surveillance—United States, 2011–2012. MMWR Suppl 2015;64(No. SS-3):1–14. PubMedexternal icon
- Painter JE, Gargano JW, Collier SA, Yoder JS. Giardiasis surveillance—United States, 2011–2012. MMWR Suppl 2015;64(No SS-3):15–25. PubMedexternal icon
- Wilson NO, Hall RL, Montgomery SP, Jones JL. Trichinellosis surveillance—United States, 2008–2012. MMWR Surveill Summ 2015;64(No. SS-1):1–8. PubMedexternal icon
- CDC. Babesiosis surveillance—18 states, 2011. MMWR Morb Mortal Wkly Rep 2012;61:505–9. PubMedexternal icon
- Council of State and Territorial Epidemiologists. Events that may constitute a public health emergency of international concern. Position statement 07-ID-06. Atlanta, GA: Council of State and Territorial Epidemiologists; 2006. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/07-ID-06.pdfpdf iconexternal icon
- World Health Organization. International Health Regulations, 2nd ed. Geneva, Switzerland: World Health Organization; 2005. http://apps.who.int/iris/bitstream/10665/43883/1/9789241580410_eng.pdfpdf iconexternal icon
- Council of State and Territorial Epidemiologists. CSTE position statement. National reporting for initial detections of novel influenza A viruses. Atlanta, GA: Council of State and Territorial Epidemiologists; 2007. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/07-ID-01.pdfpdf iconexternal icon
- Richards CL, Iademarco MF, Anderson TC. A new strategy for public health surveillance at CDC: improving national surveillance activities and outcomes. Public Health Rep 2014;129:472–6.
Corresponding author: Kimberly Thomas, Division of Health Informatics and Surveillance, Center for Surveillance, Epidemiology and Laboratory Services, CDC. Telephone: 404-639-2290; E-mail: [email protected].
 BOX 1. Infectious diseases and conditions designated by CSTE and CDC as nationally notifiable during 2015*
BOX 1. Infectious diseases and conditions designated by CSTE and CDC as nationally notifiable during 2015*
Anthrax
Arboviral diseases, neuroinvasive and nonneuroinvasive†
California serogroup virus diseases
Chikungunya virus disease
Eastern equine encephalitis virus disease
Powassan virus disease
St. Louis encephalitis virus disease
West Nile virus disease
Western equine encephalitis virus disease
Babesiosis
Botulism
Foodborne
Infant
Wound
Other
Brucellosis
Campylobacteriosis†
Chancroid
Chlamydia trachomatis infection
Cholera (toxigenic Vibrio cholerae O1 or O139)
Coccidioidomycosis
Cryptosporidiosis
Cyclosporiasis
Dengue virus infections†
Dengue
Dengue-like illness
Severe dengue
Diphtheria
Ehrlichiosis and anaplasmosis
Anaplasma phagocytophilum infection
Ehrlichia chaffeensis infection
Ehrlichia ewingii infection
Undetermined human ehrlichiosis/anaplasmosis
Giardiasis
Gonorrhea
Haemophilus influenzae, invasive disease†
Hansen’s disease (Leprosy)
Hantavirus infection, non-Hantavirus pulmonary syndrome†
Hantavirus pulmonary syndrome†
Hemolytic uremic syndrome, postdiarrheal
Hepatitis viral infections
Hepatitis A, acute
Hepatitis B, acute
Hepatitis B, chronic
Hepatitis B, perinatal infection
Hepatitis C, acute
Hepatitis C, past or present
HIV diagnoses§
Influenza-associated pediatric mortality
Invasive pneumococcal disease (Streptococcus pneumoniae, invasive disease)
Legionellosis
Leptospirosis
Listeriosis
Lyme disease
Malaria
Measles
Meningococcal disease (Neisseria meningitidis)†
Mumps
Novel influenza A virus infections
Pertussis
Plague
Poliomyelitis, paralytic
Poliovirus infection, nonparalytic
Psittacosis
Q fever
Acute
Chronic
Rabies
Human
Animal
Rubella
Rubella, congenital syndrome
Salmonellosis
Severe acute respiratory syndrome-associated coronavirus disease (SARS-CoV)
Shiga toxin-producing Escherichia coli (STEC)
Shigellosis
Smallpox
Spotted fever rickettsiosis
Streptococcal toxic shock syndrome
Syphilis¶
Syphilis, congenital†
Syphilitic stillbirth
Tetanus
Toxic shock syndrome (other than streptococcal)
Trichinellosis
Tuberculosis
Tularemia
Typhoid fever (caused by Salmonella enterica serotype typhi)
Vancomycin-intermediate Staphylococcus aureus (VISA) infection
Vancomycin-resistant Staphylococcus aureus (VRSA) infection
Varicella (morbidity)
Varicella (mortality)
Vibriosis (any species of the family Vibrionaceae, other than toxigenic Vibrio cholerae O1 or O139)
Viral hemorrhagic fever**
Crimean-Congo hemorrhagic fever virus
Ebola virus
Lassa virus
Lujo virus
Marburg virus
New World arenavirus – Guanarito virus
New World arenavirus – Junin virus
New World arenavirus – Machupo virus
New World arenavirus – Sabia virus
Yellow fever
* This list reflects position statements approved in 2014 by CSTE for national surveillance, which were implemented in January 2015. National surveillance case definitions for these infectious diseases and conditions are available at https://wwwn.cdc.gov/nndss/conditions.
† Campylobacteriosis, Chikungunya virus disease (neuroinvasive and nonneuroinvasive), and Hantavirus infection, non-Hantavirus pulmonary syndrome were added to the notifiable disease list in 2015. For the other specified conditions, the year 2015 reflects a modified surveillance case definition for the specified diseases, as per approved 2014 CSTE position statements.
§ AIDS (Acquired Immunodeficiency Syndrome) has been reclassified as HIV stage III.
¶ Includes the following categories: primary, secondary, latent (including early latent and late latent), and late syphilis with clinical manifestations (including late benign syphilis and cardiovascular syphilis).
**As of January 1, 2015, the event code for Viral Hemorrhagic Fevers (VHF) was retired and new event codes were used to report disease-specific VHF cases.
Abbreviations: OPHSS = Office of Public Health Scientific Services; NCEZID = National Center for Emerging and Zoonotic Infectious Diseases; DVBD = Division of Vector-Borne Diseases; NCHHSTP = National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention; DSTDP = Division of STD Prevention; DHCPP = Division of High Consequence Pathogens and Pathology; DVH = Division of Viral Hepatitis; DHAP = Division of HIV/AIDS Prevention; NCIRD = National Center for Infectious and Respiratory Diseases; ID = Influenza Division; DTE = Division of Tuberculosis Elimination; DVD = Division of Viral Diseases.
* An unknown case classification status is used when a reporting jurisdiction sends aggregate counts of cases or when the surveillance information system of a reporting jurisdiction does not capture case classification data. In both situations, cases are verified to meet the case classification (e.g., confirmed, probable, and suspected) specified in the publication criteria.
† Publication criteria for the National Notifiable Diseases Surveillance System (NNDSS): for a case report of a nationally notifiable disease to be published in MMWR, the reporting state or territory must have designated the disease reportable in their state or territory for the year corresponding to the year of report to CDC. After this criterion is met, the disease-specific criteria listed in Box 2 are applied. When the above-listed table indicates that all reports will be earmarked for publication, this means that cases designated with unknown or suspect case confirmation status will be published just as probable and confirmed cases will be published. Because CSTE position statements customarily are not finalized until July of each year, NNDSS data for the newly added conditions usually are not available from all reporting jurisdictions until January of the year following the approval of the CSTE position statement.
§ Based on case classification status.
¶ Publication criteria determined by reporting jurisdictions.
Highlights for 2015
Anthrax
The CDC Select Agent Program has designated Bacillus cereus biovar anthracis as a Tier 1 select agent (1). This organism has been isolated from nonhuman primates and livestock that died of an infection clinically compatible with anthrax in Central and West Africa, but has not yet been found to infect humans (2,3). The B. cereus biovar anthracis strains are similar to Bacillus anthracis in that they harbor B. anthracis virulence plasmids and are nonhemolytic. Unlike B. anthracis, however, most of the B. cereus biovar anthracis strains are motile and all are gamma-phage-resistant. The CDC Zoonoses and Select Agent Laboratory will accept specimens for molecular testing when B. cereus biovar anthracis is suspected.
- Centers for Disease Control and Prevention (CDC), Department of Health and Human Services (HHS). Possession, use, and transfer of select agents and toxins—addition of bacillus cereus Biovar anthracis to the HHS list of select agents and toxins: interim final rule and request for comments. Fed Regist 2016;81:63138–43. PubMedexternal icon
- Antonation KS, Grützmacher K, Dupke S, et al. Bacillus cereus Biovar anthracis causing anthrax in sub-Saharan Africa—chromosomal monophyly and broad geographic distribution. PLoS Negl Trop Dis 2016;10:e0004923. CrossRefexternal icon PubMedexternal icon
- Klee SR, Brzuszkiewicz EB, Nattermann H, et al. The genome of a Bacillus isolate causing anthrax in chimpanzees combines chromosomal properties of B. cereus with B. anthracis virulence plasmids. PLoS One 2010;5:e10986. CrossRefexternal icon PubMedexternal icon
Arboviral Disease, Neuroinvasive and Nonneuroinvasive
In 2015, a total of 2,175 West Nile virus (WNV) disease cases were reported, including 1,455 cases of neuroinvasive disease (e.g., meningitis, encephalitis, and acute flaccid paralysis) and 146 deaths (1). WNV disease cases were reported from 43 states and the District of Columbia. Over half (61%) of all WNV neuroinvasive disease cases were reported from California (N = 585) and Texas (N = 196). The incidence of WNV neuroinvasive disease was 0.45 cases per 100,000 population and was similar to the median incidence during 2002–2014 (median: 0.41; range: 0.13–1.02).
After WNV, the next most commonly reported causes of domestically acquired arboviral diseases were La Crosse virus, followed by St. Louis encephalitis virus, Jamestown Canyon virus, Powassan virus, and Eastern equine encephalitis virus. All cases of St. Louis encephalitis (N = 23) were reported from Arizona, which experienced a concurrent outbreak of WNV and St. Louis encephalitis virus disease (2). Jamestown Canyon virus disease cases continue to be reported from new locations (e.g., Iowa, New Jersey, Ohio, and Wyoming) following the implementation of routine Jamestown Canyon virus antibody testing at CDC in 2013 (3). Although rare, Eastern equine encephalitis virus disease remained the most severe arboviral disease, with four deaths among six patients.
A total of 896 chikungunya virus disease cases were reported from U.S. states, including one locally transmitted case from Texas (4). All other cases occurred in travelers returning from affected areas. A total of 237 chikungunya virus disease cases were reported from U.S. territories. Of these, 227 were locally transmitted cases reported from Puerto Rico and the U.S. Virgin Islands. The remaining 10 cases occurred in travelers returning from other affected areas.
- Krow-Lucal E, Lindsey NP, Lehman J, Fischer M, Staples JE. West Nile virus and other nationally notifiable arboviral diseases—United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66:51–5. CrossRefexternal icon PubMedexternal icon
- Venkat H, Krow-Lucal E, Hennessey M, et al. Notes from the field: concurrent outbreaks of St. Louis encephalitis virus and West Nile virus disease—Arizona, 2015. MMWR Morb Mortal Wkly Rep 2015;64:1349–50. PubMedexternal icon
- Pastula DM, Hoang Johnson DK, White JL, Dupuis AP 2nd, Fischer M, Staples JE. Jamestown Canyon virus disease in the United States—2000–2013. Am J Trop Med Hyg 2015;93:384–9. CrossRefexternal icon PubMedexternal icon
- CDC. Chikungunya virus: 2015 final data for the United States. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/chikungunya/geo/united-states-2015.html
Babesiosis
Babesiosis is caused by protozoan parasites of the genus Babesia, which infect red blood cells. Babesia infection can range from asymptomatic to life threatening. Clinical manifestations might include fever, chills, other nonspecific influenza-like symptoms, and hemolytic anemia. Babesia parasites usually are tickborne but also can be transmitted via blood transfusion or congenitally (1).
In 2015, a total of 2,074* cases of babesiosis were reported to CDC by 24 of the 33 states in which babesiosis was a reportable condition; 93% (1,925) of the 2,074 reported cases occurred in residents of seven states (Connecticut, Massachusetts, Minnesota, New Jersey, New York, Rhode Island, and Wisconsin). The median age of patients was 63 years (range: <1–99 years); 67% were male, 33% were female, and the sex was unknown for less than 1%. Among the 1,596 case-patients for whom data were available, 84% (1,342) had symptom onset dates during June–August.
* This number differs slightly from the denominator of 2,100 presented in the tables. At the request of the pertinent health departments, 28 erroneous reports not retracted before the deadline for finalizing the data for the tables were removed and two additional cases reported after the deadline were included.
- Herwaldt BL, Linden JV, Bosserman E, Young C, Olkowska D, Wilson M. Transfusion-associated babesiosis in the United States: a description of cases. Ann Intern Med 2011;155:509–19. CrossRefexternal icon PubMedexternal icon
Botulism
Botulism is a severe paralytic illness caused by toxins produced by Clostridium botulinum. Exposure to the toxin can occur by ingestion (foodborne botulism), in situ production from C. botulinum colonization of either a wound (wound botulism) or the gastrointestinal tract (infant botulism and adult intestinal colonization botulism), or overdose of botulinum toxin used for cosmetic or therapeutic purposes (1). In 2015, a total of 195 confirmed cases of botulism were reported, including 138 cases of infant botulism, 37 foodborne cases, and 20 cases classified as other, including wound botulism. During 2015, a total of five outbreaks (events with two or more cases) of foodborne botulism were reported. One outbreak was associated with home-canned potatoes in a potato salad (23 cases), one with fermented seal flipper (four cases), and one with beets roasted in aluminum foil and kept at room temperature (two cases). In addition, there were two outbreaks of two cases (each affected person living in the same household or facility in which the foodborne source was unknown).
All U.S. state and territorial governments maintain 24-hour telephone services for reporting of botulism and other public health emergencies. Health care providers should report suspected botulism cases immediately to their local or state health departments to obtain botulism antitoxin, which is more effective the earlier it is given, and to initiate the public health investigation into the source of botulinum toxin and prevent additional cases. In the United States, CDC maintains intensive surveillance for cases of botulism and provides consultation and antitoxin for suspected cases in children, adolescents, and adults. The California Department of Public Health provides consultation and antitoxin for suspected cases in infants. State health departments can reach the CDC botulism duty officer on call 24 hours a day, 7 days a week via the CDC Emergency Operations Center at 770-488-7100 and the California Department of Public Health botulism duty officer at 510-231-7600.
- Sobel J. Botulism. Clin Infect Dis 2005;41:1167–73. CrossRefexternal icon PubMedexternal icon
Brucellosis
During 2015, NNDSS received reports of 126 brucellosis cases in the United States. The South Atlantic, West South Central, and Pacific regions accounted for 83 of these cases, with 21, 27, and 35 cases reported, respectively. Brucellosis can be transmitted through consumption of unpasteurized dairy products or undercooked meat, inhalation, or direct contact (1). To prevent brucellosis infection, avoid consumption of unpasteurized dairy products and undercooked meat, and use proper personal protective equipment when working with Brucella in occupational settings, or when exposed to potentially infected animals. Common signs and symptoms of brucellosis include fever, sweats, malaise, anorexia, headache, fatigue, and pain in joints and muscles (2). If physicians suspect brucellosis, it is advised that they inform laboratories of this suspicion so as to minimize the risk for exposure from patient specimens and testing procedures.
- CDC. Brucellosis—transmission. Atlanta, GA: US Department of Health and Human Services, CDC: 2012. https://www.cdc.gov/brucellosis/transmission/index.html
- CDC. Brucellosis—signs and symptoms. Atlanta, GA: US Department of Health and Human Services, CDC; 2012. https://www.cdc.gov/brucellosis/symptoms/index.html
Campylobacteriosis
Campylobacteriosis became a nationally notifiable condition in 2015. The probable case definition was updated in 2015 to include cases detected by culture-independent diagnostic tests (CIDT) in addition to cases epidemiologically linked to a probable or confirmed case of campylobacteriosis. In its first year of national surveillance, the incidence of confirmed and probable campylobacteriosis was 17.7 cases per 100,000 population. Preliminary 2015 data from the Foodborne Diseases Active Surveillance Network (FoodNet), which conducts active surveillance for campylobacteriosis in 10 U.S. sites, showed an annual incidence of 17.1 culture-confirmed and CIDT-positive infections of Campylobacter per 100,000 population (1). Children aged <5 years had the highest reported national incidence rates of campylobacteriosis in 2015. Seasonality of transmission was evident, with the largest number of infections reported during June–August (2).
Campylobacter causes an estimated 1.3 million illnesses and 120 deaths annually in the United States; of these, an estimated 1 million are transmitted by food consumed in the United States (3). Campylobacter infection is commonly associated with the consumption of undercooked chicken and raw milk and usually occurs as single, sporadic cases (4), but outbreaks can occur. In 2015, a total of 35 outbreaks caused at least 280 illnesses and were linked to various sources including contaminated chicken liver pâté, grilled chicken, raw milk, and irrigation water (5).
- Huang JY, Henao OL, Griffin PM, et al. Infection with pathogens transmitted commonly through food and the effect of increasing use of culture-independent diagnostic tests on surveillance—Foodborne Diseases Active Surveillance Network, 10 U.S. sites, 2012–2015. MMWR Morb Mortal Wkly Rep 2016;65:368–71. CrossRefexternal icon PubMedexternal icon
- CDC. Foodborne Diseases Active Surveillance Network. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/foodnet/reports/data/infections.html
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
- Friedman CR, Hoekstra RM, Samuel M, et al. ; Emerging Infections Program FoodNet Working Group. Risk factors for sporadic Campylobacter infection in the United States: a case-control study in FoodNet sites. Clin Infect Dis 2004;38(Suppl 3):S285–96. CrossRefexternal icon PubMedexternal icon
- CDC. National Outbreak Reporting System FOOD Tool. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://wwwn.cdc.gov/foodborneoutbreaks
Chlamydia trachomatis Infection
Chlamydia is the most frequently reported nationally notifiable disease in the United States, with 1,526,658 cases reported to the CDC in 2015. Rates of reported cases increased during 2014–2015, with states in the South reporting the largest rates of cases. Rates were highest among females aged 20–24 years (3,764.3 cases per 100,000 females) followed by females aged 15–19 years (2,986.4 per 100,000). In 2015, the rate of reported cases of chlamydia in women aged 15–19 and 20–24 was 3.9 and 2.5 times the rate in men of the same age groups (766.5 and 1,476.8 per 100,000 males, respectively), possibly reflecting higher screening rates among women compared with men.
Cholera
Cholera continues to be rare in the United States and is most often acquired during travel in countries where toxigenic Vibrio cholerae O1 or O139 is circulating (1–3). Of the five cholera infections reported in 2015, four were travel-associated (two with travel to Haiti, one to Cuba, and one to the Philippines). The fifth case was associated with the consumption of raw shrimp imported from the Philippines.
- Steinberg EB, Greene KD, Bopp CA, Cameron DN, Wells JG, Mintz ED. Cholera in the United States, 1995–2000: trends at the end of the Twentieth Century. J Infect Dis 2001;184:799–802. CrossRefexternal icon PubMedexternal icon
- Newton AE, Heiman KE, Schmitz A, et al. Cholera in United States associated with epidemic in Hispaniola. Emerg Infect Dis 2011;17:2166–8. CrossRefexternal icon PubMedexternal icon
- Loharikar A, Newton AE, Stroika S, et al. Cholera in the United States, 2001-2011: a reflection of patterns of global epidemiology and travel. Epidemiol Infect 2015;143:695–703. CrossRefexternal icon PubMedexternal icon
Coccidioidomycosis
Coccidioidomycosis (also called Valley fever) is a fungal infection caused by inhalation of Coccidioides spp. spores present in soil. In the United States, the disease is most commonly acquired in the desert southwest and southern California. However, local acquisition has been documented as far north as south-central Washington, suggesting that exposure could occur elsewhere in arid and semi-arid portions of the western United States. Cases are routinely reported in eastern states, likely reflecting travel to areas in which disease is endemic. The disease is also endemic to parts of Central and South America.
A substantial increase in reported coccidioidomycosis occurred during 1998–2011 (1), followed by a decrease each year during 2012–2014. In 2015, reported coccidioidomycosis cases (11,072) increased by 35% compared with 2014 (8,232 cases). In Arizona (7,622 cases) and California (3,053 cases), the two states that consistently report the most cases, the percentage increase from 2014 to 2015 (36% each) was larger than the percentage increase in all other states combined (9%).
No known changes in coccidioidomycosis testing or reporting practices occurred in Arizona or California during 2015. Therefore, the increase is likely related to year-to-year changes in the environment, including rainfall and temperature. Physicians should continue to maintain a high suspicion for coccidioidomycosis in patients who live in or have traveled to areas in which the disease is endemic, and should be aware of the possibility for coccidioidomycosis outside of its previously recognized geographic range.
- CDC. Increase in reported coccidioidomycosis—United States, 1998–2011. MMWR Morb Mortal Wkly Rep 2013;62:217–21. PubMedexternal icon
Cryptosporidiosis
Approximately 90% of human cryptosporidiosis is caused by the numerous Cryptosporidium parvum and Cryptosporidium hominis subtypes. Although cryptosporidiosis affects persons of all age groups, the incidence rate of nationally notified cases is highest in children aged 1–4 years (1). A substantial increase in transmission of Cryptosporidium occurs during the summer as indicated by data on disease onset date. This seasonality coincides with increased warm-weather use of recreational water, the exposure to which is a well-established risk factor for cryptosporidiosis. Cryptosporidium has emerged as the leading cause of nationally notified recreational water–associated outbreaks and waterborne disease outbreaks overall (2003–2012) (2). Transmission through recreational water is facilitated by the substantial number (up to 108–109) of immediately infectious Cryptosporidium oocysts that can be shed in a single bowel movement (3), the extended time (days to weeks) that oocysts can be shed (4), the low (≤10 oocysts) infectious dose (5), and the extreme tolerance of Cryptosporidium oocysts to chlorine (6). In 2015, the post-2004 increase in national annual incidence continued; before 2005, the annual incidence was <1.5 cases/100,000 population and the annual case count was <4,000 cases/year. Additionally, the proportion of probable cases remained at slightly greater than one third (37%) of all cases. This likely reflects changes in the diagnostic landscape and laboratory-focused changes in the 2011 and 2012 national case definitions.
In 2015, to further elucidate Cryptosporidium transmission and thus the epidemiology of cryptosporidiosis, CDC formally launched CryptoNet, a surveillance system that integrates molecular characterization (which is needed to discriminate among species and their subtypes because conventional diagnostic tests cannot) and epidemiologic data. CryptoNet has successfully differentiated clusters of illness caused by different Cryptosporidium species and detected outbreaks caused by rare subtypes. Additional information about CryptoNet is available at https://www.cdc.gov/parasites/crypto/cryptonet.html.
In the United States, public health codes for public aquatic venues (e.g., pools, hot tubs/spas, and interactive water play areas [water playgrounds]) are written, enacted, implemented, and enforced by state or local officials. No federal agency regulates the design, construction, operation, and maintenance of these venues. To support state and local jurisdictions, CDC led the development and revision of the Model Aquatic Health Code (MAHC) (https://www.cdc.gov/mahc/editions/current.html). This guidance document integrates the recent research and best practices with specific code language and explanatory materials to minimize risk for illness and injury in public aquatic venues. MAHC recommendations particularly aim to minimize Cryptosporidium transmission. For example, MAHC recommends that public aquatic venues intended for young swimmers aged <5 years (those more likely to contaminate the water because they are more likely to have inadequate toileting and hygiene skills) should include secondary disinfection systems (e.g., ultraviolet light) to inactivate at least 99.9% of Cryptosporidium oocysts. To ensure its continued relevance, MAHC recommendations are updated every 2 years through an all-stakeholder–driven process via the Council for the Model Aquatic Health Code, taking into account the latest scientific data and aquatics sector innovations (https://ww.cmahc.org/index.phpexternal icon).
- Painter JE, Hlavsa MC, Collier SA, Xiao L, Yoder JS. Cryptosporidiosis surveillance—United States, 2011–2012. MMWR Suppl 2015;64(No. SS-3):1–14. PubMedexternal icon
- Hlavsa MC, Roberts VA, Kahler AM, et al. Outbreaks of illness associated with recreational water—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2015;64:668–72. PubMedexternal icon
- Goodgame RW, Genta RM, White AC, Chappell CL. Intensity of infection in AIDS-associated cryptosporidiosis. J Infect Dis 1993;167:704–9. CrossRefexternal icon PubMedexternal icon
- Chappell CL, Okhuysen PC, Sterling CR, DuPont HL. Cryptosporidium parvum : intensity of infection and oocyst excretion patterns in healthy volunteers. J Infect Dis 1996;173:232–6. CrossRefexternal icon PubMedexternal icon
- Chappell CL, Okhuysen PC, Langer-Curry R, et al. Cryptosporidium hominis : experimental challenge of healthy adults. Am J Trop Med Hyg 2006;75:851–7. PubMedexternal icon
- Murphy JL, Arrowood MJ, Lu X, Hlavsa MC, Beach MJ, Hill VR. Effect of cyanuric acid on the inactivation of Cryptosporidium parvum under hyperchlorination conditions. Environ Sci Technol 2015;49:7348–55. CrossRefexternal icon PubMedexternal icon
Cyclosporiasis
Of the 644* cyclosporiasis cases reported in 2015, a total of 394 (61%) were domestically acquired (i.e., they occurred in persons with no history of travel outside the United States and Canada during the 14-day incubation period), 199 (31%) were associated with international travel, and 51 (8%) occurred in persons for whom travel history was unknown or missing. Among the domestically acquired cases, at least 357 (91%) occurred in persons with illness onset during May–August. A vehicle of infection (fresh cilantro from Mexico) was identified in a multistate outbreak of 61† restaurant-associated cases in Georgia (18 cases), Texas (35 cases), and Wisconsin (8 cases) (1). A vehicle of infection was not identified for the remaining 296 (83% of 357) domestically acquired cases in persons with illness onset during May–August. Molecular typing methods, which could facilitate linkage of cyclosporiasis cases, are not yet available for C. cayetanensis.
* This number differs slightly from the denominator of 645 cases reported in the tables. One erroneous report was not retracted before the deadline for finalizing the data.
† An additional 29 probable cases were associated with this multicluster outbreak but were not reported to NNDSS or included here.
- CDC. Cyclosporiasis outbreak investigations—United States, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2015.
Dengue
Dengue is a mosquito-borne, acute febrile illness characterized by myalgia, headache, leukopenia, and minor bleeding manifestations (1). Patients with severe dengue experience plasma leakage resulting in fluid accumulation, hemorrhage, and/or major organ impairment (e.g., liver failure, myocarditis, and impaired consciousness). Dengue is endemic throughout much of the tropics and subtropics, where an estimated 50–100 million cases and 9,200 deaths occur annually (2). With proper clinical management, the case-fatality rate of hospitalized dengue patients can be <0.5% (3). Efforts to improve outcomes among persons with dengue include an online clinical education course developed by CDC (https://www.cdc.gov/dengue/training/cme.html).
In 2014, CSTE approved a modification of the case definitions for reported dengue cases effective January 1, 2015. Newly approved reporting categories were based on the World Health Organization dengue case definitions that have been in use since 2009 (1). “Dengue” is now used for patients that met the clinical case definition for dengue (i.e., fever and one of: nausea/vomiting, rash, aches and pains, positive tourniquet test, leukopenia, or any warning sign for severe dengue). “Dengue-like illness” indicates patients with fever and either clinical suspicion or diagnostic evidence of dengue, but not meeting the clinical case definition for dengue. “Severe dengue,” which includes the prior categorizations of dengue hemorrhagic fever and dengue shock syndrome, is used for patients that meet the clinical case definition for severe dengue: severe plasma leakage, severe bleeding, or severe organ involvement. Laboratory definitions are also modified in that detection of antidengue virus IgM antibody by ELISA is considered confirmatory if the patient lives in or recently traveled to an area without evidence of circulation of any other flavivirus.
In 2015, a total 951 laboratory-positive cases were reported from 48 of the 50 states, two of the five territories, and the District of Columbia. Most (72%) cases were travel-associated, and case-patients most frequently had a history of travel to the Caribbean or Americas, where chikungunya and Zika viruses had recently emerged. Because dengue, chikungunya, and Zika virus disease often have a similar clinical presentation, the moderate number of reported dengue cases compared with previous years, despite low levels of dengue cases detected in areas of the Caribbean and the Americas where the disease is endemic, might be attributable to increased diagnostic testing to differentiate between these diseases. The states or jurisdictions with the most travel-associated dengue cases reported were California (138), Florida (81), New York City (74), New Jersey (57), and Texas (30). Hawaii reported a large outbreak of dengue, in which 200 locally acquired dengue cases were detected in Hawaii residents that live on or had traveled to Oahu. Florida reported one locally acquired dengue case, and was the only other state to report a locally acquired dengue case in 2015. Reports of laboratory-positive dengue cases were at historic lows in the dengue-endemic Caribbean territories of Puerto Rico and the U.S. Virgin Islands (58 and 3 cases, respectively). Sixteen cases of dengue-like illness and six cases of severe dengue were reported in 2015, all in travelers and none in residents of U.S. territories.
- World Health Organization. Dengue: guidelines for diagnosis, treatment, prevention and control. Geneva, Switzerland: World Health Organization; 2009.
- Stanaway JD, Shepard DS, Undurraga EA, et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. Lancet Infect Dis 2016;16:712–23. CrossRefexternal icon PubMedexternal icon
- Lam PK, Tam DT, Diet TV, et al. Clinical characteristics of Dengue shock syndrome in Vietnamese children: a 10-year prospective study in a single hospital. Clin Infect Dis 2013;57:1577–86. CrossRefexternal icon PubMedexternal icon
Diphtheria
Respiratory diphtheria, a vaccine-preventable disease, is rare in the United States, and no cases were reported during 2015. Since 2003, two cases have been reported to CDC: a probable case in 2012, and a confirmed case caused by nontoxigenic C. diphtheriae in 2014. Children and adults should be vaccinated according to the schedule recommended by the Advisory Committee on Immunization Practices (1). Ensuring and sustaining high childhood vaccination coverage rates above 90% and high coverage with decennial booster doses in adolescents and adults are required for herd protection in the population.
- CDC. General recommendations on immunization—recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2011;60(No. RR-2):1–64. PubMedexternal icon
Ehrlichiosis and Anaplasmosis
Ehrlichiosis and anaplasmosis are rickettsial tickborne diseases that have been notifiable since 1998 (1). The principal vectors of Anaplasma phagocytophilum include the blacklegged tick (Ixodes scapularis) and the Western blacklegged tick (Ixodes pacificus) (2). The number of reported cases of anaplasmosis increased by approximately 31%, from 2,800 cases in 2014 to 3,656 cases in 2015. This change represents the largest increase in reported cases of anaplasmosis since the disease became notifiable in 1998. Most notably, the number of cases in the New England and the Mid-Atlantic regions increased by 22% and 70%, respectively. The lone star tick (Amblyomma americanum) transmits both Ehrlichia chaffeensis and Ehrlichia ewingii to humans (2). The number of reported cases of Ehrlichia chaffeensis (1,288) and Ehrlichia ewingii (14) were similar to the previous year (1,475 and 17, respectively). Changes in reported cases might indicate a dynamic change in reporting practices, an increase in awareness, and an increase in the use of diagnostic assays.
- Council of State and Territorial Epidemiologists. Adding ehrlichiosis as a condition reportable to the National Public Health Surveillance System. Atlanta, GA: Council of State and Territorial Epidemiologists; 1998. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/1998–ID-6.pdfpdf iconexternal icon
- CDC. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States: a practical guide for health care and public health professionals. MMWR Recomm Rep 2016;65(No. RR-2).
Giardiasis
Giardiasis is the most common enteric parasitic infection in the United States, infecting an estimated 1.2 million persons annually (1). Symptomatology is variable, but giardiasis is normally characterized by diarrhea, abdominal cramps, bloating, weight loss, and malabsorption; extraintestinal symptoms are possible (2). Infected persons can shed Giardia for several weeks, and recent studies indicate potential for chronic sequelae from giardiasis (3). Giardia is endemic worldwide, including in the United States, and is the most commonly diagnosed pathogen among travelers returning to the United States from other countries (4). Giardia is commonly detected in internationally adopted children screened in the United States; often, these children do not have gastrointestinal symptoms (5). In 2015, the reported incidence of giardiasis appears to have stabilized compared with 2014. Giardia is transmitted through the fecal-oral route with the ingestion of environmentally stable Giardia cysts. Most information on giardiasis transmission is from outbreak investigations; 242 giardiasis outbreaks reported to CDC for 1971–2011 resulted from waterborne (74.8%), foodborne (15.7%), person-to-person (2.5%), and animal contact (1.2%) transmission (6). On the basis of outbreak trends, investigators identified groundwater and distribution system vulnerabilities in drinking water systems, inadequate pool disinfection, fruit and vegetable contamination, and poor food handler hygiene as possible targets for giardiasis prevention measures. However, most reported giardiasis cases are not linked to known outbreaks. Among reported cases, <2% are documented as outbreak-associated (7). An ecological study of sporadic giardiasis in the United States indicated that high county-level reliance on private wells was associated with higher giardiasis rates (8). Prospective epidemiologic studies and continued outbreak and case surveillance are needed to understand transmission pathways and to identify effective public health prevention measures.
Population studies of Giardia seroprevalence would contribute substantially to understanding the prevalence of giardiasis in the United States (9). Enhanced genotyping methods would increase knowledge of the molecular epidemiology of Giardia, including elucidating species-specific subassemblages (10). Application of these tools to epidemiologic studies and surveillance has the potential to improve understanding of giardiasis risk factors, enable researchers to identify outbreaks by linking cases currently classified as sporadic infections, and provide risk factor information needed to inform prevention strategies.
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
- Cantey PT, Roy S, Lee B, et al. Study of nonoutbreak giardiasis: novel findings and implications for research. Am J Med 2011;124:1175.e1–8. CrossRefexternal icon PubMedexternal icon
- Hanevik K, Wensaas KA, Rortveit G, Eide GE, Mørch K, Langeland N. Irritable bowel syndrome and chronic fatigue 6 years after giardia infection: a controlled prospective cohort study. Clin Infect Dis 2014;59:1394–400. CrossRefexternal icon PubMedexternal icon
- Harvey K, Esposito DH, Han P, et al. . Surveillance for travel-related disease—GeoSentinel Surveillance System, United States, 1997–2011. MMWR Surveill Summ 2013;62(No. SS-3):1–23. PubMedexternal icon
- Staat MA, Rice M, Donauer S, et al. Intestinal parasite screening in internationally adopted children: importance of multiple stool specimens. Pediatrics 2011;128:e613–22. PubMedexternal icon
- Adam EA, Yoder JS, Gould H, Hlavsa MC. Giardiasis outbreaks in the United States, 1971–2011. Epidemiol Infect 2016. https://www.ncbi.nlm.nih.gov/pubmed/26750152external icon
- Schnell K, Collier S, Derado G, Yoder J, Gargano JW. Giardiasis in the United States—an epidemiologic and geospatial analysis of county-level drinking water and sanitation data, 1993–2010. J Water Health 2016;14:267–79. PubMedexternal icon
- Yoder JS, Gargano JW, Wallace RM, Beach MJ. Giardiasis surveillance—United States, 2009-2010. MMWR Surveill Summ 2012;61(No. SS-5):13–23. PubMedexternal icon
- Priest JW, Moss DM, Visvesvara GS, Jones CC, Li A, Isaac-Renton JL. Multiplex assay detection of immunoglobulin G antibodies that recognize Giardia intestinalis
and Cryptosporidium parvum antigens. Clin Vaccine Immunol 2010;17:1695–707. CrossRefexternal icon PubMedexternal icon - Feng Y, Xiao L. Zoonotic potential and molecular epidemiology of Giardia species and giardiasis. Clin Microbiol Rev 2011;24:110–40. CrossRefexternal icon PubMedexternal icon
Haemophilus influenzae Disease
The epidemiology of invasive Haemophilus influenzae disease has changed in the United States in the post-Haemophilus influenzae type b (Hib) vaccine era. Since the introduction of conjugate Hib vaccines in 1987, the incidence of invasive Hib disease among children aged <5 years decreased by 99% (1); in 2015, incidence was 0.15 cases per 100,000 children. However, rates of Hib disease among American Indian/Alaskan Native (AI/AN) children remain much higher than among non-AI/AN children. During 2015, nontypeable Haemophilus influenzae caused the majority of invasive disease in all age groups.
To ensure appropriate chemoprophylaxis measures for contacts of invasive Hib disease and to detect emergence of invasive non-Hib disease, serotyping of all Haemophilus influenzae isolates in children aged <5 years, and thorough and timely investigation of all cases of Hib disease, are essential (2,3).
- MacNeil JR, Cohn AC, Farley M, et al. Current epidemiology and trends in invasive Haemophilus influenzae disease—United States, 1989–2008. Clin Infect Dis 2011;53:1230–6. CrossRefexternal icon PubMedexternal icon
- Briere EC, Rubin L, Moro PL, Cohn A, Clark T, Messonnier N. Prevention and control of haemophilus influenzae type b disease: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 2014;63(No. RR-1):1–14. PubMedexternal icon
- CDC. Best practices for use of PCR for diagnosing Haemophilus influenzae and Neisseria meningitidis and importance of identifying serotype/serogroup. Atlanta, GA: US Department of Health and Human Diseases, CDC; 2016. https://www.cdc.gov/meningococcal/laboratory/pcr-guidance-mening-hflu.html
Hansen’s Disease (Leprosy)
In 2015, a total of 89 cases of Hansen’s Disease (HD) were reported to NNDSS from 21 states. HD is not reportable in all states; therefore, the number of cases reported annually to NNDSS will likely be lower than those reported to the National Hansen’s Disease Program, which is responsible for providing patient treatment for all patients in the United States (1). Approximately 67% of the 82 cases with known sex reported were male. Of the 81 cases with reported age, 55 (68%) were aged ≥40 years. Of the states that reported HD cases, the majority of the 89 new cases reported were from Florida (29 [33%]), Texas (20 [22%]), California (7 [8%]), and Hawaii (7 [8%]). The number of cases reported by Florida, Texas, and California all increased from the previous year while the number of cases reported by Hawaii decreased by 50%. In addition, the number of cases reported from Guam increased by nine cases from 2014 to 22 cases.
- US Department of Health and Human Services. Hansen’s disease data and statistics. Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration; 2016. https://www.hrsa.gov/hansensdisease/dataandstatistics.htmlexternal icon
Hantavirus Pulmonary Syndrome
Hantavirus pulmonary syndrome (HPS) is an acute, severe pulmonary disease characterized by pulmonary edema following a nonspecific prodrome (1). National surveillance for hantavirus infections in the United States began in 1993 during an outbreak of severe respiratory illness in the Four Corners region, and HPS became nationally notifiable in 1995. The presence of fever and pulmonary symptoms in a patient with laboratory-confirmed evidence of hantavirus infection is required for a HPS case to be reported through NNDSS (2).
Laboratory-confirmed cases of hantavirus infection that had nonspecific viral symptoms (e.g. fever, chills, myalgia, headache, gastrointestinal symptoms) and did not develop into HPS (“non-pulmonary hantavirus infection”) have been described (3–5). It is believed that HPS is the more frequently observed clinical presentation, although the rarity of the disease and the potential for missed diagnoses of nonpulmonary hantavirus infection with nonspecific clinical symptoms makes it difficult to estimate accurately the number of hantavirus infections. In 2014, CSTE resolved to expand the national reporting of laboratory confirmed hantavirus infections to include HPS and nonpulmonary hantavirus infection (6). The first year of reporting of nonpulmonary hantavirus cases was 2015, and three nonpulmonary cases were reported in addition to 21 HPS cases.
- MacNeil A, Nichol ST, Spiropoulou CF. Hantavirus pulmonary syndrome. Virus Res 2011;162:138–47. CrossRefexternal icon PubMedexternal icon
- Knust B, Rollin PE. Twenty-year summary of surveillance for human hantavirus infections, United States. Emerg Infect Dis 2013;19:1934–7. CrossRefexternal icon PubMedexternal icon
- Núñez JJ, Fritz CL, Knust B, et al. ; Yosemite Hantavirus Outbreak Investigation Team. Hantavirus infections among overnight visitors to Yosemite National Park, California, USA, 2012. Emerg Infect Dis 2014;20:386–93. CrossRefexternal icon PubMedexternal icon
- Kitsutani PT, Denton RW, Fritz CL, et al. Acute Sin Nombre hantavirus infection without pulmonary syndrome, United States. Emerg Infect Dis 1999;5:701–5. CrossRefexternal icon PubMedexternal icon
- Armstrong LR, Bryan RT, Sarisky J, et al. Mild hantaviral disease caused by Sin Nombre virus in a four-year-old child. Pediatr Infect Dis J 1995;14:1108–09. CrossRefexternal icon PubMedexternal icon
- CDC. Nationally Notifiable Diseases Surveillance System, hantavirus infection, non-hantavirus pulmonary syndrome 2015 case definition. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. http://wwwn.cdc.gov/nndss/conditions/hantavirus-infection-non-hantavirus-pulmonary-syndrome/case-definition/2015
Hemolytic Uremic Syndrome
Hemolytic uremic syndrome (HUS) is characterized by the triad of hemolytic anemia, thrombocytopenia, and renal insufficiency. The most common etiology of postdiarrheal HUS in the United States is infection with Shiga toxin-producing Escherichia coli (STEC), principally STEC O157:H7 (1,2). Children aged <5 years progress to HUS more often than all other persons infected with STEC O157:H7 (15.3% vs. 6.3%) (3). In 2015, as in previous years, the age group with the most reported cases to NNDSS was children aged 1‒4 years (122 of 274 cases).
- Banatvala N, Griffin PM, Greene KD, et al. ; Hemolytic Uremic Syndrome Study Collaborators. The United States National Prospective Hemolytic Uremic Syndrome Study: microbiologic, serologic, clinical, and epidemiologic findings. J Infect Dis 2001;183:1063–70. CrossRefexternal icon PubMedexternal icon
- Mody RK, Luna-Gierke RE, Jones TF, et al. Infections in pediatric postdiarrheal hemolytic uremic syndrome: factors associated with identifying shiga toxin-producing Escherichia coli. Arch Pediatr Adolesc Med 2012;166:902–9. CrossRefexternal icon PubMedexternal icon
- Gould LH, Demma L, Jones TF, et al. Hemolytic uremic syndrome and death in persons with Escherichia coli O157:H7 infection, foodborne diseases active surveillance network sites, 2000–2006. Clin Infect Dis 2009;49:1480–5. CrossRefexternal icon PubMedexternal icon
Human Immunodeficiency Virus Diagnoses
CDC requires states to transmit HIV case data via the enhanced HIV/AIDS Reporting System (eHARS), which is a browser-based system deployed at 54 state/local and territorial public health departments in the United States. HIV surveillance data are not reported through NNDSS. De-identified data are transmitted monthly from health departments, through the secure access management services (SAMS), directly to CDC’s Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, and are incorporated into the National HIV Surveillance System database.
By April 2008, all 50 states, the District of Columbia, and six U.S. dependent areas had laws or regulations requiring confidential name-based reporting for human immunodeficiency virus (HIV) infection, in addition to reporting persons whose disease has been classified as stage 3 (acquired immunodeficiency syndrome [AIDS]). In 2008, CDC published a revised surveillance case definition for HIV infection that includes AIDS and incorporates the HIV infection classification (1). Laboratory-confirmed evidence of HIV infection is required to meet the surveillance case definition for HIV infection, including stage 3 (AIDS). In 2014, the HIV surveillance case definition was revised again to adapt to changes in diagnostic criteria used by laboratories and clinicians (2). The laboratory criteria for defining a confirmed case of HIV infection were changed to accommodate multitest algorithms that do not include previously required tests (e.g., Western blot). New to the case definition was the inclusion of criteria for differentiating HIV-1 and HIV-2 infections and for recognizing early HIV infection (stage 0), during which viral loads might be high enough and CD4 T-lymphocyte counts low enough to be mistaken for stage 3 (AIDS). In addition, the revised definition consolidated the staging systems for adults/adolescents and children, simplified surveillance criteria for opportunistic illnesses indicative of stage 3, and incorporated revisions of clinical criteria (i.e., medical record documentation) for reporting diagnoses without laboratory evidence.
Because retroactive implementation of some features (e.g., the new staging system) of the 2014 case definition was impractical, the following criteria were used to classify cases in this report (1): cases diagnosed before 2014 were classified according to the 2008 HIV case definition and (2) cases diagnosed in 2014 and 2015 were classified according to the 2014 HIV case definition.
A total of 33,817 cases of HIV infection were diagnosed in the United States during 2015 and reported to CDC as of December 2015. Blacks/African Americans had the highest rate of diagnoses of HIV infection of all racial/ethnic groups (37.7 per 100,000) and accounted for 44.5% of diagnoses in 2015; whites and Hispanics/Latinos followed, accounting for 27.8% and 22.8% of diagnoses, respectively. Although HIV affects persons in all age groups, cases were most frequently diagnosed in adults aged 25–39 years. Areas with the highest rates (≥15.0 per 100,000) of diagnoses during 2015 were the District of Columbia, Florida, Louisiana, Maryland, Mississippi, New York, and South Carolina.
- Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep 2008;57(No. RR-10):1–12. PubMedexternal icon
- CDC. Revised surveillance case definition for HIV infection—United States, 2014. MMWR Recomm Rep 2014;63(No. RR-3):1–10. PubMedexternal icon
Influenza-Associated Pediatric Mortality
In 2004, CSTE added influenza-associated pediatric mortality to the list of conditions reportable to NNDSS (1). A pediatric influenza-associated death is defined for surveillance purposes as a death resulting from a clinically compatible illness that was confirmed to be influenza by an appropriate laboratory or rapid diagnostic test in a person aged <18 years. From January 4, 2015 to January 2, 2016,* a total of 130 influenza-associated pediatric deaths were reported to CDC from 39 states and New York City.
Of the 130 influenza-associated pediatric deaths reported to CDC during 2015, two deaths occurred during the 2013–14 influenza season, 122 deaths occurred during the 2014–15 influenza season, and six occurred during the 2015–16 influenza season. An influenza season spans the time period between MMWR week 40 of a calendar year to MMWR week 39 of the following year. Ninety-three (72%) were associated with influenza A viruses, 35 (27%) with influenza B viruses, one (1%) with an influenza virus for which the type was not determined, and one (1%) death was associated with influenza A virus and influenza B virus co-infection. Of 93 influenza A viruses, subtype was determined for 54 (58%); three were influenza A (H1N1) pdm09 viruses and 51 were influenza A (H3N2) viruses.
Among the 130 deaths reported in 2015, a total of 16 children (12%) were aged <6 months, 46 (35%) were aged 6–59 months, 39 (30%) were aged 5–11 years, and 29 (22%) were aged 12–17 years; the median age at the time of death was 5.4 years (range: 27 days–17 years). The median age in 2015 is similar to previous influenza seasons during nonpandemic periods, but is lower than the median age of deaths observed during the 2009 pandemic.
Information on the location of death was available for 128 (98.5%) of the 130 children: 80 (63%) children died after being admitted to the hospital (73 were admitted to the intensive care unit), 22 (17%) died in the emergency department, and 26 (20%) died outside the hospital. Information on pre-existing medical conditions was reported for 127 (98%) children: 55 (43%) children had one or more underlying medical condition known to confer increased risk for complications from influenza (2). The most common group of underlying conditions was neurologic disorders (e.g., moderate to severe developmental delay, seizure disorders, cerebral palsy, mitochondrial disorders, neuromuscular disorders, and neurologic conditions), which was reported for 23 (18%) of 127 children. Eighteen (14%) children had chromosomal abnormalities and/or genetic syndromes, 17 (13%) had a chronic pulmonary condition (e.g., asthma, cystic fibrosis, or other chronic pulmonary disease), and 13 (10%) had cardiac disease or congenital heart disease.
Among the 130 deaths in children, 73 children had specimens collected for bacterial culture from normally sterile sites (e.g., blood, pleural fluid, cerebrospinal fluid, and lung tissue). Of these, 35 (48%) had positive cultures, and six (17%) of the 35 were positive for more than one pathogen. Staphylococcus aureus was detected in 15 (43%) of 35 positive cultures; nine were methicillin-resistant, one was methicillin-sensitive, and for five specimens methicillin-sensitivity testing was not done. Three cultures (9%) were positive for Streptococcus pneumoniae, three (9%) were positive for Group A Streptococcus, two cultures (6%) were positive for Pseudomonas aeruginosa, and two cultures (6%) were positive for Streptococcus species. Other bacterial pathogens identified included one each with Enterobacter cloacoe, Enterococcus avium, Klebsiella pneumonia, and Stenotrophomonas maltophilia.
Of 89 children aged ≥6 months at the time of illness onset for whom seasonal vaccination status was known, 27 (30%) had been fully vaccinated against influenza as recommended by the Advisory Committee on Immunization Practices (2,3). Twenty-one children were aged <6 months at the time of their illness onset and therefore considered ineligible for vaccination.
Influenza seasons typically span portions of 2 calendar years and can vary widely in terms of severity and timing of peak activity, thus affecting the number of deaths reported in a calendar year. The 2014–15 influenza season was moderately severe and peaked in late December 2014, with predominant circulation of antigenically and genetically drifted influenza A (H3N2) viruses (4). Continued surveillance for influenza-associated mortality is important to monitor the effects of seasonal and novel influenza, factors contributing to severe influenza-associated disease, and the influence of interventions among children.
* For 2015, MMWR only included influenza-associated pediatric deaths that were reported from MMWR week 1 through MMWR week 52 (January 4, 2015–January 2, 2016).
- Council of State and Territorial Epidemiologists. Influenza-associated pediatric mortality. Position statement 04-ID-04. Atlanta, GA: Council of State and Territorial Epidemiologists. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/04-ID-04-FINAL.pdfpdf iconexternal icon
- Grohskopf LA, Olsen SJ, Sokolow LZ, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP) — United States, 2014–15 influenza season. MMWR Morb Mortal Wkly Rep 2014;63:691–7. PubMedexternal icon
- Grohskopf LA, Sokolow LZ, Olsen SJ, Bresee JS, Broder KR, Karron RA. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2015–16 influenza season. MMWR Morb Mortal Wkly Rep 2015;64:818–25. CrossRefexternal icon PubMedexternal icon
- Appiah GD, Blanton L, D’Mello T, et al. Influenza activity—United States, 2014–15 season and composition of the 2015–16 influenza vaccine. MMWR Morb Mortal Wkly Rep 2015;64:583–90. PubMedexternal icon
Legionellosis
In 2015, a total of 6,079 cases of Legionellosis were reported in the United States (1.89 cases per 100,000 persons of all ages). The rate of reported cases continues to rise. Several high-profile outbreaks of Legionnaires’ disease occurred in 2015, including an outbreak of 138 cases in the South Bronx, New York City, which was the largest community-associated outbreak since the 1976 Philadelphia outbreak that led to the discovery of Legionella.
Because Legionella transmission occurs from human-made environmental settings, the most effective strategy for the prevention of Legionnaires’ disease is through control of Legionella in building water systems. In 2015, ASHRAE (formerly known as the American Society of Heating, Refrigerating, and Air-Conditioning Engineers) published a consensus industry standard for reducing the risk for Legionnaires’ disease called ASHRAE 188 (1). This document calls for the development and implementation of water management programs in large or complex building water systems. It is based on best practices and focuses on identifying hazardous conditions and applying control measures to interrupt Legionella amplification and transmission. The CDC and its partners developed a toolkit to facilitate implementation of this industry standard (2).
- ASHRAE. Legionellosis: risk management for building water systems. ANSI/ASHRAE Standard 188. Atlanta, GA: ASHRAE; 2015. https://www.ashrae.orgexternal icon
- CDC. Developing a water management program to reduce Legionella growth and spread in buildings: a practical guide to implementing industry standards. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/legionella/WMPtoolkit
Leptospirosis
In 2015, a total of 10 states, jurisdictions, and territories reported 96 leptospirosis cases. Puerto Rico reported the highest number of leptospirosis cases (45), followed by Hawaii (22) and Guam (11). Among the 40 cases reported from U.S. states and jurisdictions (territories excluded), 95% (38/40) were male, and a temporal peak of 10 cases was seen in August, with cases reported by five states and jurisdictions that month.
NNDSS began receiving case notifications for leptospirosis in 2014. In the first two years of notifications combined (2014–2015), the total case count for leptospirosis was 203 cases reported from 17 states, jurisdictions, and territories, with 114 total cases reported from Puerto Rico, 45 from Hawaii, and 11 from Guam. Comparatively, individual states and jurisdictions in the continental United States reported six or fewer cases over the 2-year period. Leptospirosis is not reportable in 14 states.
Leptospirosis, one of the most widespread zoonotic diseases, is caused by pathogenic species of the Leptospira genus. There are 22 Leptospira species, 10 of which are pathogenic, including more than 250 serovars known to cause disease (1,2). Most commercially available tests include polymerase chain reaction (PCR) and serology using qualitative Immunoglobulin M (IgM)-based assays. While PCR is a confirmatory test, IgM-based assays are considered screening tests and should ideally be confirmed with the microscopic agglutination test (MAT). MAT is the gold standard for leptospirosis serology, with acute infection confirmed by either a four-fold increase in titers between acute and convalescent sera or a single titer greater than or equal to 1:800. MAT can be performed at select reference laboratories around the country, including CDC. Culture is also confirmatory, however, this method is less commonly used because the bacteria is fastidious, requires specialized media, and might take several months to grow. The benefit of culture is the ability to perform various serovar identification techniques using the grown isolate. Although MAT is useful for confirming leptospirosis cases, it is not recommended for identifying the infecting serovar because of frequent cross-reaction between serovars (3). In 2014 and 2015, only 37% (40/107) and 49% (47/96) of leptospirosis cases, respectively, were reported as confirmed. Laboratory confirmation of probable leptospirosis cases is encouraged.
Disease presentation can vary from a mild, influenza-like illness to a severe and fatal disease with multiorgan failure. The nonspecific acute, febrile illness presentation of leptospirosis cases mimics that of many other infectious diseases, which can make initial recognition difficult. Continued efforts to increase awareness of leptospirosis in health care providers is needed to improve detection and reporting of the disease. If leptospirosis is suspected, treatment should be initiated early in the course of illness and not delayed while awaiting laboratory confirmation, as this might reduce the severity of the disease.
- Bourhy P, Collet L, Brisse S, Picardeau M. Leptospira mayottensis sp. nov ., a pathogenic species of the genus Leptospira isolated from humans. Int J Syst Evol Microbiol 2014;64:4061–7. CrossRefexternal icon PubMedexternal icon
- Haake D, Levett P. Leptospira species (Leptospirosis). In: Bennett J, Dolin R, Blaser M, eds. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 8th ed. Philadelphia, PA: Elsevier Inc.; 2015: 2714–20.
- Levett PN. Usefulness of serologic analysis as a predictor of the infecting serovar in patients with severe leptospirosis. Clin Infect Dis 2003;36:447–52. CrossRefexternal icon PubMedexternal icon
Listeriosis
Listeria monocytogenes infection (listeriosis) is rare but can cause severe invasive disease (e.g., bacteremia and meningitis). Listeriosis is predominately acquired through contaminated food and occurs most frequently among older adults, persons with certain immunocompromising conditions, and pregnant women and their newborns. Pregnancy-associated listeriosis can manifest as a relatively mild illness for the woman, but can result in fetal loss or severe neonatal disease.
Listeriosis has been nationally notifiable since 2000. In 2015, the incidence of listeriosis reported to NNDSS was 0.24 infections per 100,000 population. Progress toward the 2020 national target of 0.20 infections per 100,000 population (1) is measured through the Foodborne Diseases Active Surveillance Network (FoodNet), which conducts active, population-based surveillance for listeriosis in 10 U.S. states. FoodNet reported a preliminary annual incidence of Listeria monocytogenes in 2015 of 0.24 infections per 100,000 population, the same rate nationally reported through NNDSS (2).
The Listeria Initiative is an enhanced surveillance system designed to aid in the rapid investigation of listeriosis outbreaks by combining L. monocytogenes isolate molecular subtyping and whole-genome sequencing (WGS) results with epidemiologic data collected by state and local health departments (3). As part of the Listeria Initiative, CDC recommends that all clinical isolates of L. monocytogenes be forwarded routinely to a public health laboratory for pulsed-field gel electrophoresis (PFGE) subtyping and WGS, and that these results be submitted to PulseNet, the National Molecular Subtyping Network for Foodborne Disease Surveillance (4). In addition, communicable disease programs are asked to interview all patients with listeriosis promptly using the standard Listeria Initiative questionnaire, which is available in English and Spanish (https://www.cdc.gov/listeria/surveillance.html).
Beginning in September 2013, whole genome sequencing has been performed on all clinical isolates as part of a project conducted by CDC, state and local health departments, the Food and Drug Administration, the U.S. Department of Agriculture’s Food Safety and Inspection Service, the National Institutes of Health, and international partners (5,6). All isolate sequences are deposited in publicly available databases at the National Center for Biotechnology Information of the National Institutes of Health. The Listeria Initiative has aided in the timely identification and removal of contaminated food during several listeriosis investigations, including the first multistate outbreak linked to commercially produced ice cream in the U.S., causing 10 illnesses (7).
- US Department of Health and Human Services. Healthy people 2020 objectives. Washington, DC: US Department of Health and Human Services; 2017. https://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=14external icon
- Huang JY, Henao OL, Griffin PM, et al. Infection with pathogens transmitted commonly through food and the effect of increasing use of culture-independent diagnostic tests on surveillance—Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2012–2015. MMWR Morb Mortal Wkly Rep 2016;65:368–71. CrossRefexternal icon PubMedexternal icon
- CDC. National Enteric Disease Surveillance: the Listeria Initiative. Atlanta, Georgia: US Department of Health and Human Services, CDC; 2014. https://www.cdc.gov/listeria/pdf/ListeriaInitiativeOverview_508.pdfpdf icon
- CDC. PulseNet. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https:/www.cdc.gov/pulsenet
- Jackson BR, Tarr C, Strain E, et al. Implementation of nationwide real-time whole-genome sequencing to enhance listeriosis outbreak detection and investigation. Clin Infect Dis 2016;63:380–6. CrossRefexternal icon PubMedexternal icon
- Carleton HA, Gerner-Smidt P. Whole-genome sequencing is taking over foodborne disease surveillance. Microbe 2016;11:311–7.
- CDC. Multistate outbreak of listeriosis linked to Blue Bell Creameries products (final update). Atlanta, GA: US Department of Health and Human Services, CDC; 2015. https://www.cdc.gov/listeria/outbreaks/ice-cream-03-15/index.html
Lyme Disease
In 2015, a total of 38,069 confirmed and probable cases of Lyme disease were reported to CDC, an increased number compared with the number reported annually between 2010 and 2014; however, cases did not surpass the number reported in 2009, the year with the highest case counts. The geographic distribution of high incidence areas with Lyme disease appears to be expanding based on data reported to NNDSS. The number of counties with an incidence of ≥10 confirmed cases per 100,000 persons increased from 324 in 2008 to 424 in 2015.
Measles
Measles was declared eliminated from the United States in 2000. Since then, elimination has been maintained through high population immunity along with adequate disease surveillance and public health response capacity (1,2). Nonetheless, because measles remains endemic in much of the world, importations continue to result in sporadic cases and outbreaks in the United States, which can be costly to control (3). As in recent years, the majority of measles cases (97%) were import-associated (i.e., cases that are internationally imported, epidemiologically linked to an imported case, or for which viral genetic evidence indicates an imported genotype) in 2015 (4).
A measles outbreak is defined as a chain of transmission involving three or more cases. Six outbreaks occurred in 2015, accounting for 80% of the total (n = 150) cases. The largest outbreak originated in California in late December 2014, and was linked to two Disney theme parks (5,6). Cases were reported through early March 2015, including 113 cases reported in 2015. The outbreak spread to seven other U.S. states (Arizona, Colorado, Nebraska, Oregon, Texas, Utah, and Washington), and two bordering countries (Mexico and Canada) (6). The majority of measles cases associated with outbreaks in 2015 occurred in persons who were unvaccinated or whose vaccination status was unknown (5).
In the spring of 2015, an adult with a suppressed immune system died from pneumonia related to an undetected measles infection. One or two out of 1,000 persons with measles in the United States will die, even with the best supportive care. This measles case underscores the fact that the disease can cause serious complications and that immunocompromised persons are at higher risk for these complications.
- Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr 2014;168:148–55. CrossRefexternal icon PubMedexternal icon
- Fiebelkorn AP, Redd SB, Gastañaduy PA, et al. A comparison of postelimination measles epidemiology in the United States, 2009–2014 versus 2001–2008. J Pediatric Infect Dis Soc 2017;6:40–8. PubMedexternal icon
- Ortega-Sanchez IR, Vijayaraghavan M, Barskey AE, Wallace GS. The economic burden of sixteen measles outbreaks on United States public health departments in 2011. Vaccine 2014;32:1311–7. CrossRefexternal icon PubMedexternal icon
- Council of State and Territorial Epidemiologists. Revision of measles, rubella, and congenital syndrome case classification as part of elimination goals in the United States. Position statement 2006-ID-16. Atlanta, GA: Council of State and Territorial Epidemiologists; 2006.
- Clemmons NS, Gastañaduy PA, Fiebelkorn AP, Redd SB, Wallace GS. Measles—United States, January 4–April 2, 2015. MMWR Morb Mortal Wkly Rep 2015;64:373–6. PubMedexternal icon
- Zipprich J, Winter K, Hacker J, Xia D, Watt J, Harriman K. Measles outbreak—California, December 2014–February 2015. MMWR Morb Mortal Wkly Rep 2015;64:153–4. PubMedexternal icon
Meningococcal Disease
Meningococcal disease is a serious and life-threatening infection, with a case-fatality ratio of 10%–15%; survivors often lose limbs or suffer brain damage. In 2015, rates of meningococcal disease continued to be at historic lows in the United States (0.12 cases per 100,000 population); however, during 2015, two outbreaks of serogroup B meningococcal disease occurred on college campuses in the United States, resulting in nine cases and one death. In 2015, CDC’s Advisory Committee on Immunization Practices (ACIP) recommended routine use of serogroup B meningococcal (MenB) vaccine in certain groups at increased risk for disease, including use during outbreaks of serogroup B meningococcal disease (1). ACIP also recommended that a MenB vaccine series may be administered to adolescents and young adults aged 16–23 years to provide short-term protection against most strains of serogroup B meningococcal disease (2). The preferred age for serogroup B meningococcal vaccination is age 16–18 years (2).
- Folaranmi T, Rubin L, Martin SW, Patel M, MacNeil JR. Use of serogroup B meningococcal (MenB) vaccines in persons aged ≥10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2015. MMWR Morb Mortal Wkly Rep 2015;64:608–12. PubMedexternal icon
- MacNeil JR, Rubin L, Folaranmi T, Ortega-Sanchez IR, Patel M, Martin SW. Use of serogroup B meningococcal (MenB) vaccines in adolescents and young adults: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2015. MMWR Morb Mortal Wkly Rep
2015;64:1171–6. CrossRefexternal icon PubMedexternal icon
Mumps
A total of 1,329 mumps cases in the United States were reported during 2015 from 38 states, with the majority being from three states (Illinois, Iowa, and New York). Of these 1,329 cases, 705 (53%) came from eight outbreaks of 20 or more cases. The majority (88%) of the outbreaks occurred in close-contact settings including universities, high schools and athletic teams; 83% of the large outbreak case-patients were fully vaccinated.
Outbreaks of mumps among university settings are known to occur despite high 2-dose vaccine coverage (1). The reported vaccine-effectiveness for mumps vaccine is 78% for 1-dose and 88% for 2-doses (2). Close and prolonged contact likely facilitates mumps transmission.
- Dayan GH, Quinlisk MP, Parker AA, et al. Recent resurgence of mumps in the United States. N Engl J Med 2008;358:1580–9. CrossRefexternal icon PubMedexternal icon
- McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(No. RR-4):1–34. PubMedexternal icon
Novel Influenza A Virus Infections
In 2007, CSTE added human infection with a novel influenza A virus to the list of conditions reportable to NNDSS (1). Novel influenza A virus infections are human infections with influenza A viruses that are different from currently circulating human seasonal influenza viruses. These viruses include those that are subtyped as nonhuman in origin and those that cannot be subtyped with standard methods and reagents used for currently circulating influenza viruses.
Influenza viruses that normally circulate in swine are called swine influenza viruses when isolated from swine, but are called variant viruses when isolated from humans. During 2005–2015, all reported novel influenza A human infections in the United States involved variant viruses rather than avian-origin influenza viruses. Although most persons identified with variant influenza virus infection report contact with swine preceding their illness, suggesting swine-to-human spread, limited human-to-human transmission of these viruses has occurred (2). Because the implications of ongoing transmission of these novel viruses between humans are potentially severe, prompt and thorough investigation of human infections with novel influenza viruses is critical so that the potential public health risk can be more fully understood and appropriate public health measures can be taken (3).
In 2015, seven human infections with novel influenza A viruses were reported from five states (Iowa [one], Michigan [one], Minnesota [three], New Jersey [one], and Ohio [one]) (4–6). Four of these infections were associated with influenza A (H1N2) variant viruses (H1N2v) and three with influenza A (H3N2) variant viruses (H3N2v). The median age of patients was 27 years (range: 6–43 years), and six (85.7%) were male. Reported symptoms associated with infection were fever (85.7%), cough (85.7%), fatigue (42.9%), shortness of breath (71.4%), muscle aches (28.6%), and vomiting or diarrhea (57.1%); six (85.7%) cases reported influenza-like illness (e.g. fever (≥100°F [37.8°C] with cough and/or sore throat). Three (42.9%) cases had an underlying medical condition known to confer increased risk for complications from influenza (7). All seven patients sought health care for their illness and five (71.4%) were hospitalized. Six (85.7%) patients fully recovered from their illness and one patient died from complications of their infection. Four patients reported direct contact with (e.g., touching or handling) or proximity to (e.g., walking through an area or coming within 6 feet of) swine in the week preceding illness onset. Three patients worked, lived, or visited areas near where swine were housed, but no direct contact with swine in the week before illness onset was reported. No likely human-to-human transmission of novel influenza A viruses was identified.
Variant virus infections usually occurs among persons with direct, unprotected contact with swine or environments where swine are or have been present (e.g., agricultural fairs, farms, and petting zoos). CDC conducts year-round surveillance for human infections with novel influenza A viruses in conjunction with state and local public health laboratories and conducts extensive epidemiologic investigations on each report of human infection with a novel influenza virus. Any specimen with results suggestive of a novel influenza A virus infection or that cannot be subtyped using standard methods and reagents at a public health laboratory should be immediately submitted to CDC for further testing.
- Council of State and Territorial Epidemiologists. Public health reporting and national notification for novel influenza A virus infection. Position statement 13-ID-14. Atlanta, GA: Council of State and Territorial Epidemiologists; 2012. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/13-ID-14.pdfpdf iconexternal icon
- Jhung MA, Epperson S, Biggerstaff M, et al. Outbreak of variant influenza A(H3N2) virus in the United States. Clin Infect Dis 2013;57:1703–12. CrossRefexternal icon PubMedexternal icon
- Richards S, Glazier M, Masterson K, et al. Update: Influenza A (H3N2)v transmission and guidelines—five states, 2011. MMWR Morb Mortal Wkly Rep 2012;60:1741–4. PubMedexternal icon
- Blanton L, Kniss K, Smith S, et al. Update: influenza activity—United States and worldwide, May 24–September 5, 2015. MMWR Morb Mortal Wkly Rep 2015;64:1011–6. CrossRefexternal icon PubMedexternal icon
- Appiah GD, Blanton L, D’Mello T, et al. Influenza activity—United States, 2014–15 season and composition of the 2015–16 influenza vaccine. MMWR Morb Mortal Wkly Rep 2015;64:583–90. PubMedexternal icon
- Davlin SL, Blanton L, Kniss K, et al. Influenza activity—United States, 2015–16 season and composition of the 2016–17 influenza vaccine. MMWR Morb Mortal Wkly Rep 2016;65:567–75. CrossRefexternal icon PubMedexternal icon
- Grohskopf LA, Sokolow LZ, Broder KR, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices—United States, 2016–17 influenza season. MMWR Recomm Rep 2016;65(No. RR-5):1–54. CrossRefexternal icon
Pertussis
Reported pertussis incidence decreased 37.9% from 2014 (incidence: 10.3 per 100,000 population) to 2015 (6.5 per 100,000 population). Although overall reporting declined, pertussis incidence varies geographically, and 11 states reported increases in incidence, with two states (Washington and West Virginia) reporting more than double the number of cases they reported during 2014. The highest incidence of reported pertussis continues to be observed among infants aged <1 year (67.2 per 100,000 population); however, the greatest proportion of reported pertussis cases is contributed by adolescents aged 11–19 years (32%), likely the result of waning immunity among adolescents exclusively vaccinated with acellular pertussis vaccines (1–3). Six pertussis-related deaths were reported through NNDSS during 2015. Three deaths occurred among infants aged <3 months, and the remaining were reported from adolescents and adults with co-morbidities. Two of the three pertussis-related deaths among infants aged <3 months had known maternal Tdap status, and neither mother received Tdap during the recommended 27–36 weeks of gestation. Vaccinating women with Tdap during the third trimester of every pregnancy remains the primary recommendation for preventing pertussis among young infants (4).
- Misegades LK, Winter K, Harriman K, et al. Association of childhood pertussis with receipt of 5 doses of pertussis vaccine by time since last vaccine dose, California, 2010. JAMA 2012;308:2126–32. CrossRefexternal icon PubMedexternal icon
- Skoff TH, Martin SW. Impact of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccinations on reported pertussis cases among those 11 to 18 years of age in an era of waning pertussis immunity: a follow-up analysis. JAMA Pediatr 2016;170:453–8. CrossRefexternal icon PubMedexternal icon
- Acosta AM, DeBolt C, Tasslimi A, et al. Tdap vaccine effectiveness in adolescents during the 2012 Washington State pertussis epidemic. Pediatrics 2015;135:981–9. CrossRefexternal icon PubMedexternal icon
- CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep 2013;62:131–5. PubMedexternal icon
Plague
Plague is a fulminant, life-threatening zoonosis caused by the bacterium Yersinia pestis. Transmission to humans usually occurs through the bite of an infected rodent flea and less commonly through direct contact with tissues or inhalation of respiratory secretions from infected animals. Clinical presentation varies according to the route of infection, with bubonic plague being the most common. Bubonic and septicemic plague cannot be transmitted from person to person; however, persons with pneumonic plague can transmit Y. pestis via respiratory droplets (1).
In 2015, a total of 16 confirmed cases of plague were reported to CDC, the most since 2006; four cases were fatal. Cases were reported from residents of eight states: Arizona (two cases), California (one case), Colorado (four cases), Georgia (one case), Michigan (one case), New Mexico (four cases), Oregon (two cases), and Utah (one case). Two of the confirmed cases were linked to exposures in or near Yosemite National Park, the site of a plague epizootic in 2015 (2,3).
- Inglesby TV, Dennis DT, Henderson DA, et al. ; Working Group on Civilian Biodefense. Plague as a biological weapon: medical and public health management. JAMA 2000;283:2281–90. CrossRefexternal icon PubMedexternal icon
- Kwit N, Nelson C, Kugeler K, et al. Human plague—United States, 2015. MMWR Morb Mortal Wkly Rep 2015;64:918–9. CrossRefexternal icon PubMedexternal icon
- Danforth M, Novak M, Petersen J, et al. Investigation of and response to 2 plague cases, Yosemite National Park, California, USA, 2015. Emerg Infect Dis 2016;22. CrossRefexternal icon PubMedexternal icon
Rabies
During 2015, all 50 states reported a total of 5,491 rabid animals to CDC (1), representing a 9.1% decrease from the 6,033 rabid animals in 2014 (2). Two human rabies deaths occurred in 2015 (1,3), compared with one human rabies death reported in 2014. Of the 5,491 cases of animal rabies, 4,983 (90.7%) involved wildlife. Increases in the number of animals reported rabid were observed for the following species: foxes (4.5%), and dogs (13.6%) (1). Decreases in the number of animals reported rabid were observed for the following species: bats (3%), cats (10.3%), raccoons (11%), and skunks (14%) (1). There were no significant changes in the number of rabid cattle reported from 2014. Other reported rabid wildlife included six bobcats (Lynx rufus), 15 coyotes (Canis latrans), six deer (presumably Odocoileus virginianus), two opossums (Didelphis virginiana), two otters (presumably Lontra canadensis), one elk (Cervus elaphus), and one ringtail (Bassariscus astutus) (1). Rabid rodents and lagomorphs reported in 2015 included 25 groundhogs (Marmota monax), six rabbits (not specified), one squirrel (not specified), and two beavers (Castor canadensis) (1). There was a 4.1% decrease in the number of samples submitted for rabies testing in 2015 as compared with 2014. Two human rabies deaths occurred in 2015 (1,3). The first was a male aged 65 years in Massachusetts who was bitten by a dog while abroad. The second involved a female aged 77 years in Wyoming who had contact with a bat.
- Birhane MG, Cleaton JM, Monroe BP, et al. Rabies surveillance in the United States during 2015. J Am Vet Med Assoc 2017;250:1117–30. CrossRefexternal icon PubMedexternal icon
- Monroe BP, Yager P, Blanton J, et al. Rabies surveillance in the United States during 2014. J Am Vet Med Assoc 2016;248:777–88. CrossRefexternal icon PubMedexternal icon
- Harrist A, Styczynski A, Wynn D, et al. Human rabies—Wyoming and Utah, 2015. MMWR Morb Mortal Wkly Rep 2016;65:529–33. CrossRefexternal icon PubMedexternal icon
Salmonellosis
In 2015, the incidence of salmonellosis in the United States was 17.2 laboratory-confirmed infections per 100,000 population, one and a half times the 2020 national health objectives target of 11.4 (1). Data from the Foodborne Diseases Active Surveillance Network (FoodNet), which conducts active surveillance for salmonellosis in 10 U.S. sites, showed a preliminary annual incidence of Salmonella of 15.9 in 2015, slightly lower than the rate reported to NNDSS (2). During 2015, as in previous years of surveillance, children aged <5 years had the highest reported incidence rate of salmonellosis. Salmonellosis is reported most frequently in late summer and early fall; in 2015, this seasonality was evident, with most reported infections occurring during July–October.
Salmonella causes an estimated 1.2 million illnesses annually in the United States; of these, an estimated 1 million are transmitted by food consumed in the United States (3). Salmonella can contaminate a wide range of foods, and different serotypes tend to have different animal reservoirs and food sources, making control challenging. The largest multistate outbreak of Salmonella infections in 2015 (serotype Poona) was traced to imported cucumbers; other notable outbreaks in 2015 were linked to small turtles (serotypes Sandiego and Poona), pork (serotypes I 4,[5],12:i:- and Infantis), live poultry (serotypes Enteritidis, Hadar, Indiana and Muenchen), raw, frozen, stuffed chicken entrees (serotype Enteritidis), frozen raw tuna (serotypes Paratyphi B variant L[+] tartrate[+] and Weltevreden), pet crested geckos (serotype Muenchen), and raw sprouted nut butter spreads (serotype Paratyphi B variant L[+] tartrate[+]) (4).
- US Department of Health and Human Services. Healthy people 2020 objectives. Washington, DC: US Department of Health and Human Services; 2017. https://www.healthypeople.gov/2020/topics-objectives/topic/food-safety/objectives?topicId=14external icon
- CDC. Foodborne Diseases Active Surveillance Network. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/foodnet/reports/data/infections.html
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
- CDC. Reports of selected salmonella outbreak investigations, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. https://www.cdc.gov/salmonella/outbreaks-2015.html
Shiga toxin-producing Escherichia coli (STEC)
In 2015, the incidence of laboratory-confirmed Shiga toxin-producing Escherichia coli (STEC) infections in the United States was 2.2 cases per 100,000 population. Preliminary data from FoodNet, an active, population-based surveillance system for enteric diseases, reported culture-confirmed STEC incidence of 2.6 in 2015 (1). As in previous years of FoodNet surveillance, the age group with the highest incidence of reported STEC infections was children aged 1–4 years (8.0 per 100,000 population). In 2015, multistate outbreaks of STEC infection were linked to rotisserie chicken salad (STEC O157:H7) and multiple outbreaks linked to an unidentified food or ingredient served at several locations of a national Mexican chain restaurant (STEC O26) (2).
Public health actions to monitor, prevent, and control STEC infections are based on serogroup characterization. Development of postdiarrheal hemolytic uremic syndrome (HUS), a severe complication of STEC infection, is most strongly associated with STEC O157. Non-O157 STEC, a diverse group that varies in virulence, comprises approximately 50 other serogroups. Increased use of culture-independent diagnostic tests in recent years has led to increased detection and reporting of non-O157 STEC infection (3,4). STEC produces Shiga toxins (Stx): Stx1, Stx2, or both. In general, strains that produce certain types of Stx2 are the most virulent (5). Accounting for underdiagnosis, an estimated 96,000 illnesses are caused by STEC O157 and 168,000 illnesses by non-O157 STEC each year (6,7).
Stool specimens from patients with community-acquired diarrhea submitted to clinical laboratories should be tested routinely both by culture for STEC O157 and by an assay that detects Shiga toxins (or the genes that encode them). Detection of Shiga toxin alone is inadequate for clinical management and public health investigation; characterizing STEC isolates by serogroup and by pulsed-field gel electrophoresis pattern is important to detect, investigate, and control outbreaks.
- CDC. Foodborne Diseases Active Surveillance Network. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/foodnet/reports/data/infections.html
- CDC. Reports of selected E. coli outbreak investigations from 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2015. https://www.cdc.gov/ecoli/2015-outbreaks.html
- Gould LH, Mody RK, Ong KL, et al. ; Emerging Infections Program Foodnet Working Group. Increased recognition of non-O157 Shiga toxin-producing Escherichia coli infections in the United States during 2000–2010: epidemiologic features and comparison with E. coli O157 infections. Foodborne Pathog Dis 2013;10:453–60. CrossRefexternal icon PubMedexternal icon
- Iwamoto M, Huang JY, Cronquist AB, et al. Bacterial enteric infections detected by culture-independent diagnostic tests—FoodNet, United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015;64:252–7. PubMedexternal icon
- Mody RK, Griffin PM. Fecal shedding of Shiga toxin-producing Escherichia coli : what should be done to prevent secondary cases? Clin Infect Dis 2013;56:1141–4. CrossRefexternal icon PubMedexternal icon
- Heiman KE, Mody RK, Johnson SD, Griffin PM, Gould LH. Escherichia coli O157 Outbreaks in the United States, 2003–2012. Emerg Infect Dis 2015;21:1293–301. CrossRefexternal icon PubMedexternal icon
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
Shigellosis
In 2015, the probable case definition of shigellosis was updated to include cases detected by culture-independent diagnostic tests (CIDT) in addition to cases epidemiologically linked to a probable or confirmed case of shigellosis. Incidence of shigellosis reported in the United States during 2015 was 7.3 culture-confirmed and CIDT-positive infections per 100,000 population. Preliminary 2015 data from the Foodborne Diseases Active Surveillance Network (FoodNet), which conducts active surveillance for shigellosis in 10 U.S. sites, showed an annual incidence of 6.5 culture-confirmed and CIDT-positive infections of Shigella per 100,000 population (1). As in previous years, the highest number of reported cases of shigellosis in 2015 occurred among children aged <10 years. Shigellosis does not demonstrate marked seasonality, likely reflecting the contribution of year-round person-to-person transmission.
Adjusting for underdiagnosis, Shigella causes an estimated 500,000 illnesses annually in the United States (2). Shigella is most often transmitted person-to-person, including through sexual contact between men who have sex with men (MSM), and also can be transmitted by contaminated food or contaminated water used for drinking or recreational purposes (3–5). Childcare-associated outbreaks are common and are often difficult to control (6). Homeless persons (4) and international travelers (7,8) are also at higher risk for infection.
Shigella species have caused multidrug-resistant outbreaks in the United States (8–10). In 2014, the National Antimicrobial Resistance Monitoring System (NARMS) reported that among Shigella isolates tested for resistance to first-line antimicrobial agents, 2.4% were resistant to ciprofloxacin and 4.7% were resistant to azithromycin; 15.3% of isolates were resistant to at least ampicillin and trimethoprim-sulfamethoxazole (11). MSM and HIV-infected persons appear to be at greater risk for antibiotic resistant Shigella infections than the general adult population (9,10,12,13).
When shigellosis is suspected, clinicians should obtain a relevant clinical history, including sexual history in sexually active patients; collect stool specimens for laboratory testing; base treatment, if indicated, on results of antimicrobial susceptibility; and counsel patients about prevention.
- Huang JY, Henao OL, Griffin PM, et al. Infection with pathogens transmitted commonly through food and the effect of increasing use of culture-independent diagnostic tests on surveillance—Foodborne Diseases Active Surveillance Network, 10 U.S. sites, 2012–2015. MMWR Morb Mortal Wkly Rep 2016;65:368–71. CrossRefexternal icon PubMedexternal icon
- Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
- Gupta A, Polyak CS, Bishop RD, Sobel J, Mintz ED. Laboratory-confirmed shigellosis in the United States, 1989-2002: epidemiologic trends and patterns. Clin Infect Dis 2004;38:1372–7. CrossRefexternal icon PubMedexternal icon
- Hines JZ, Pinsent T, Rees K, et al. Shigellosis outbreak among men who have sex with men and homeless persons—Oregon, 2015–2016. MMWR Morb Mortal Wkly Rep 2016;65:812–3. CrossRefexternal icon PubMedexternal icon
- Baker KS, Dallman TJ, Ashton PM, et al. Intercontinental dissemination of azithromycin-resistant shigellosis through sexual transmission: a cross-sectional study. Lancet Infect Dis
2015;15:913–21. CrossRefexternal icon PubMedexternal icon - Arvelo W, Hinkle CJ, Nguyen TA, et al. Transmission risk factors and treatment of pediatric shigellosis during a large daycare center-associated outbreak of multidrug resistant Shigella sonnei : implications for the management of shigellosis outbreaks among children. Pediatr Infect Dis J 2009;28:976–80. CrossRefexternal icon PubMedexternal icon
- Gray MD, Lampel KA, Strockbine NA, Fernandez RE, Melton-Celsa AR, Maurelli AT. Clinical isolates of Shiga toxin 1a-producing Shigella flexneri with an epidemiological link to recent travel to Hispañiola. Emerg Infect Dis 2014;20:1669–77. CrossRefexternal icon PubMedexternal icon
- Bowen A, Hurd J, Hoover C, et al. Importation and domestic transmission of Shigella sonnei
resistant to ciprofloxacin—United States, May 2014–February 2015. MMWR Morb Mortal Wkly Rep 2015;64:318–20. PubMedexternal icon - Heiman KE, Karlsson M, Grass J, et al. Notes from the field: Shigella with decreased susceptibility to azithromycin among men who have sex with men—United States, 2002–2013. MMWR Morb Mortal Wkly Rep 2014;63:132–3. PubMedexternal icon
- Bowen A, Eikmeier D, Talley P, et al. Notes from the field: outbreaks of Shigella sonnei
infection with decreased susceptibility to azithromycin among men who have sex with men—Chicago and Metropolitan Minneapolis-St. Paul, 2014. MMWR Morb Mortal Wkly Rep
2015;64:597–8. PubMedexternal icon - CDC. National Antimicrobial Resistance Monitoring System for enteric bacteria (NARMS): human isolates surveillance report for 2014 (final report). Atlanta, GA: US Department of Health and Human Services, CDC; 2016.
- Bowen A, Grass J, Bicknese A, Campbell D, Hurd J, Kirkcaldy RD. Elevated risk for multidrug-resistant Shigella infections among men who have sex with men—United States, 2011–2015. Emerg Infect Dis 2016;22:1613–6. CrossRefexternal icon PubMedexternal icon
- Chiou CS, Izumiya H, Kawamura M, et al. The worldwide spread of ciprofloxacin-resistant Shigella sonnei among HIV-infected men who have sex with men, Taiwan. Clin Microbiol Infect. 2016;22(4):383 e11–6.
Spotted Fever Rickettsiosis
Spotted fever group rickettsioses are a group of diseases caused by closely related bacteria in the genus Rickettsia. These bacteria are spread to humans through the bite of infected arthropods, primarily ticks. Incidence of spotted fever rickettsioses rose 12% between 2014 and 2015 to the second highest level ever reported. American Indians continue to be disproportionately impacted by spotted fever rickettsioses. In 2015, incidence of spotted fever rickettsiosis among American Indians was more than twice that of whites, nine times higher than blacks, and 25 times higher than Asians and Pacific Islanders. Epidemics of Rocky Mountain spotted fever have been ongoing since 2003 on tribal lands of Arizona (1). High incidence in this region might contribute to the disproportionate burden of spotted fever rickettsiosis in American Indian populations.
- Demma LJ, Traeger MS, Nicholson WL, et al. Rocky Mountain spotted fever from an unexpected tick vector in Arizona. N Engl J Med 2005;353:587–94. CrossRefexternal icon PubMedexternal icon
Trichinellosis
In 2015, a total of 13* cases of trichinellosis were reported to CDC (10 confirmed and three probable). A known or suspected source of Trichinella infection was documented for 10 (77%) of these cases, and included bear (seven), commercial pork (one), pork from an unspecified source (one), and pork consumed during international travel (one).
Two outbreaks of trichinellosis were reported in 2015. The first outbreak included one confirmed and two probable cases in persons from Texas who reportedly consumed meat from a black bear hunted in Alaska. CDC’s laboratory detected Trichinella larvae in a sample of the leftover bear meat via microscopy. The second outbreak included two confirmed and one probable case (one confirmed and one probable from Colorado and one confirmed from Idaho), in persons who also reportedly consumed meat from a bear hunted in Alaska. Persons in both outbreaks reported cooking the bear meat via open-fire roasting or barbecue. The best way to prevent Trichinella infection is to thoroughly cook all meats to the USDA-recommended temperatures (as verified with a food thermometer) before consumption (1).
* This number differs from the denominator of 14 cases presented in tables below; one case from Wisconsin was reclassified as suspect from confirmed after the deadline for finalizing data.
- CDC. Trichinellosis: prevention and control. Atlanta, GA: US Department of Health and Human Services, CDC; 2013. https://www.cdc.gov/parasites/trichinellosis/prevent.html
Tuberculosis
Tuberculosis (TB) is one of the world’s most common deadly airborne diseases. In 2015, an estimated 10.4 million persons worldwide had TB, and 1.4 million died from the disease (1). In 2014, an estimated 1.7 billion persons worldwide had latent TB infection (LTBI), which can later develop into active disease (2). Over one million persons were granted permanent U.S. residency in 2015, approximately one-third of whom were from countries identified as having a high burden of TB disease (3). CDC and the U.S. Preventive Services Task Force recommend screening persons who have lived in countries with a high burden of TB disease for LTBI (4).
In the United States, new cases of TB disease have been reported annually since 1953 to CDC’s National Tuberculosis Surveillance System (NTSS) (5). CDC receives data from 60 reporting jurisdictions (all 50 U.S. states, the District of Columbia, New York City, and eight U.S.-affiliated islands) through a standardized data collection form, the Report of Verified Case of Tuberculosis (RVCT). In 2009, the RVCT was revised, and NTSS transitioned into an online reporting system. TB case rates remained at approximately 3.0 cases/100,000 persons each year during 2013–2015 (5). For the first time since 1992, TB cases increased by 1.6% from 9,406 cases in 2014 to 9,557 in 2015 (5).
Among all TB cases in the United States, members of racial and ethnic minorities, especially persons who were born in countries with higher TB incidence than the United States, are disproportionately affected. In 2015, 66.4% (6,350 of 9,557) of persons with TB in the United States were foreign-born. Asians comprised 33.2% (3,177 of 9,557) of all cases and 47.8% (3,033 of 6,350) of cases among foreign-born persons. In 2015, the TB rate among Asians (18.2 per 100,000 persons) was 30 times as high as the rate (0.6) among non-Hispanic whites (5).
TB drug resistance continues to be a major concern. During 1996–2015, the percentage of primary multidrug-resistant (MDR) TB cases (i.e., cases in patients with no previous history of TB disease and with a Mycobacterium tuberculosis isolate that was resistant to at least isoniazid [INH] and rifampin [RIF]) has fluctuated between 0.9% and 1.3% each year. The percentage of U.S.-born patients with primary MDR TB has remained <1.0%. However, of the total number of reported primary MDR-TB cases, the percentage occurring among foreign-born persons increased from 25.3% (103/407 persons) in 1993 to 86.3% (63/73 persons) in 2015, which is similar to the proportion in 2014. In addition, 16 extensively drug-resistant (XDR) TB cases (i.e., patients with isolates resistant to INH and RIF, plus resistance to any fluoroquinolone and at least one of three injectable second-line anti-TB drugs) have been reported since 2009 (5).
For TB elimination (<1 case/1,000,000 population) to be acheived (6), intensified efforts are needed to address the persistent disparities that exist in populations with a high risk for TB disease. Improved awareness, testing, and treatment of LTBI and TB disease among minorities and foreign-born populations are essential parts of these efforts. CDC is collaborating with partners in efforts to enhance TB testing, monitoring, and treatment of LTBI to prevent its progression to TB disease and accelerate the decrease in TB cases.
- World Health Organization. Global tuberculosis report 2016. Geneva, Switzerland: World Health Organization; 2016. http://www.who.int/tb/publications/global_report/enexternal icon
- Houben RM, Dodd PJ. The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med 2016;13:e1002152. CrossRefexternal icon PubMedexternal icon
- US Department of Homeland Security. 2015 yearbook of immigration statistics, table 3. Persons obtaining lawful permanent resident status by region and country of birth: fiscal years 2013 to 2015. https://www.dhs.gov/immigration-statistics/yearbook/2015/table3external icon
- Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force. Screening for latent tuberculosis infection in adults. JAMA 2016;316:962–9. CrossRefexternal icon PubMedexternal icon
- CDC. Reported tuberculosis in the United States, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/tb/statistics/reports/2015/default.htm
- CDC. Division of Tuberculosis Elimination strategic plan 2016–2020. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2015. https://www.cdc.gov/tb/about/strategicplan.htm
Tularemia
Tularemia is a zoonotic disease caused by the bacterium Francisella tularensis. Transmission to humans occurs through the bite of infected ticks or deer flies, direct contact with tissues of sick or dead animals, ingestion of contaminated water or undercooked meat, or inhalation of contaminated aerosols, including aerosols generated during laboratory procedures (1).
In 2015, a total of 314 tularemia cases were reported to CDC, the largest number since 1964 and a 74% increase relative to 2014. The majority of cases were reported from eight states: Arkansas (24 cases), Colorado (52 cases), Kansas (34 cases), Missouri (29 cases), Nebraska (25 cases), Oklahoma (23 cases), South Dakota (25 cases), and Wyoming (21 cases). A disproportionate increase in cases was noted in Colorado, Nebraska, South Dakota and Wyoming, possibly related to increased rabbit populations (2).
- Dennis DT, Inglesby TV, Henderson DA, et al. ; Working Group on Civilian Biodefense. Tularemia as a biological weapon: medical and public health management. JAMA 2001;285:2763–73. CrossRefexternal icon PubMedexternal icon
- Pedati C, House J, Hancock-Allen J, et al. Notes from the field: increase in human cases of tularemia—Colorado, Nebraska, South Dakota, and Wyoming, January–September 2015. MMWR Morb Mortal Wkly Rep 2015;64:1317–8. CrossRefexternal icon PubMedexternal icon
Typhoid
Typhoid fever is rare in the United States. Since 2009, an annual average of fewer than 400 cases has been reported. In 2015, a total of 367 cases were reported. Approximately 86% of U.S. cases are associated with international travel, and the risk for infection is highest for travelers visiting friends and relatives in countries where typhoid fever is endemic, especially in southern Asia, where 82% of patients with typhoid travelled within 30 days preceding their illness (1). These persons might stay for extended periods and are less likely than other travelers to seek pretravel vaccination and to observe strict safe water and food practices, perhaps due to misperception of disease risk (2). Travelers face a risk for typhoid fever when visiting even for a short time areas where the disease is endemic (3) and should consult guidelines for prevention of typhoid at https://wwwnc.cdc.gov/travel/diseases/typhoid. Paratyphoid fever, although caused by different organisms and not nationally notifiable, is an illness similar to typhoid fever and is of similar concern to travelers in regions where the disease is endemic. There is no vaccine available for paratyphoid fever (1).
- Date KA, Newton AE, Medalla F, et al. Changing patterns in enteric fever incidence and increasing antibiotic resistance of enteric fever isolates in the United States, 2008–2012. Clin Infect Dis 2016;63:322–9. CrossRefexternal icon PubMedexternal icon
- Angell SY, Cetron MS. Health disparities among travelers visiting friends and relatives abroad. Ann Intern Med 2005;142:67–72. CrossRefexternal icon PubMedexternal icon
- Steinberg EB, Bishop R, Haber P, et al. Typhoid fever in travelers: who should be targeted for prevention? Clin Infect Dis 2004;39:186–91. CrossRefexternal icon PubMedexternal icon
Varicella
Important declines in varicella incidence occurred during the first nine years of implementation of the 2-dose varicella vaccination program (1–3). Based on reports of varicella cases to CDC through NNDSS, varicella incidence has declined 85% from an average of 25.4 per 100,000 in 2005–2006 (the end of the 1-dose varicella vaccination program) to 3.8 per 100,000 in 2015. Statistically significant declines in incidence were reported for all age groups during this time, with the largest declines among children aged 5–9 years (91%) and 10–14 years (89%). During the same period, the number of states reporting varicella cases has increased from 27 in 2005 to 40 in 2015.
Varicella-specific variables important for monitoring impact of the varicella vaccination program include age, vaccination status, disease severity (e.g., number of lesions), outcome of the case (e.g., hospitalized), and whether the case is associated with an outbreak. In 2015, 96% (9,455/9,789) of cases reported to CDC from 38 states had data on at least one of the above mentioned varicella-specific variables. Of the 9,455 cases, completeness of reporting for these variables ranged from a low of 8% (n=780) for whether the case resulted in hospitalization to a high of 98% (n = 9,299) for age; completeness for other key variables was 53% (n = 4,982) for vaccination status, 43% (n = 4,028) for disease severity, and 68% (n=6,464) for whether the case was associated with an outbreak.
Among the 9,299 cases with data on age, 49% (4,553) were in persons 1–9 years, 20% (1,930) were in persons aged 10–19 years, and 21% (1,984) were in persons aged ≥20 years. Among cases for which information on vaccination status was available (n = 4,982), 58% (n = 2,900) of reported cases were in patients who had received at least 1 dose of varicella vaccine, and of those reported cases who received at least 1 dose of vaccine and had information on number of varicella doses received (n = 2,207), 57% (1,261) had received 2 doses. Mild disease (<50 lesions) was reported in 50% (2,008/4,028) of cases; 5% (36/780) of cases resulted in hospitalization; and 22% (1,446/6,464) of cases were associated with outbreaks. Less than one third of total reported cases had specimens tested for varicella (29%; 1,305/4,491), but 83% (1,086/1,305) of cases with testing were laboratory confirmed as varicella.
States are working to improve reporting of cases and completeness of varicella-specific variables (3), which will strengthen the use of national surveillance in monitoring the impact of the varicella vaccination program. Although states are sending varicella-specific data to CDC, findings describing patient characteristics should be interpreted with caution given the large proportion of missing data. Finally, increased testing of suspect cases of varicella will also improve reliability of varicella surveillance data.
- Bialek SR, Perella D, Zhang J, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics 2013;132:e1134–40. CrossRefexternal icon PubMedexternal icon
- Leung J, Lopez AS, Blostein J, et al. Impact of the US two-dose Varicella Vaccination Program on the epidemiology of varicella outbreaks: data from nine states, 2005–2012. Pediatr Infect Dis J 2015;34:1105–9. CrossRefexternal icon PubMedexternal icon
- Lopez AS, Zhang J, Marin M. Epidemiology of varicella during the 2-dose Varicella Vaccination Program—United States, 2005–2014. MMWR Morb Mortal Wkly Rep 2016;65:902–5. CrossRefexternal icon PubMedexternal icon
Vibriosis
Vibriosis, defined as infection caused by a species from the family Vibrionaceae other than toxigenic Vibrio cholerae O1 or O139, is associated with consumption of seafood, primarily raw oysters, or direct exposure to salt water, marine wildlife, or seafood drippings. Although most infections result in mild gastrointestinal illness or skin infection, severe illness or death is possible and occurs more often in those with pre-existing conditions such as liver disease, immunodeficiency, or decreased stomach acid levels (1,2).
The incidence of vibriosis has shown an overall increase since becoming a nationally notifiable disease in 2007 (3). Cases reported to NNDSS increased from 0.25 cases per 100,000 in 2007 to 0.42 cases per 100,000 population in 2015. The Foodborne Diseases Active Surveillance Network (FoodNet), which conducts active, population-based surveillance for vibriosis in 10 U.S. states also reported an increase in incidence from 0.24 per 100,000 in 2007 to a preliminary incidence of 0.39 per 100,000 population in 2015 (4). Incidence of vibriosis reported to FoodNet is used to track progress towards the Healthy People 2020 goal for vibriosis of 0.2 cases per 100,000 population (5). Of the 1,323 vibriosis cases reported to NNDSS, 386 (29.2%) were reported from Gulf coast states, and 374 (28.3%) were reported from Pacific coast states.
- Iwamoto M, Ayers T, Mahon BE, Swerdlow DL. Epidemiology of seafood-associated infections in the United States. Clin Microbiol Rev 2010;23:399–411. CrossRefexternal icon PubMedexternal icon
- Dechet AM, Yu PA, Koram N, Painter J. Nonfoodborne Vibrio infections: an important cause of morbidity and mortality in the United States, 1997–2006. Clin Infect Dis 2008;46:970–6. CrossRefexternal icon PubMedexternal icon
- Newton A, Kendall M, Vugia DJ, Henao OL, Mahon BE. Increasing rates of vibriosis in the United States, 1996–2010: review of surveillance data from 2 systems. Clin Infect Dis 2012;54(Suppl 5):S391–5. CrossRefexternal icon PubMedexternal icon
- Huang JY, Henao OL, Griffin PM, et al. Infection with pathogens transmitted commonly through food and the effect of increasing use of culture-independent diagnostic tests on surveillance—Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2012–2015. MMWR Morb Mortal Wkly Rep 2016;65:368–71. CrossRefexternal icon PubMedexternal icon
- US Department of Health and Human Services. Healthy people 2020. FS-1.6 data details: reduce infections caused by Vibrio species transmitted commonly through food. Washington, DC: US Department of Health and Human Services, 2017. https://www.healthypeople.gov/node/4480/data_detailsexternal icon
Viral Hemorrhagic Fever
Viral Hemorrhagic Fever (VHF) is a group of acute febrile illnesses that are caused by over 30 viruses (1). Nationally notifiable VHFs are those with documented person to person transmission, such as: Crimean-Congo hemorrhagic fever, Ebola virus disease (EVD), Lassa fever, Lujo, Marburg, and several New World Arenaviruses (Junin, Machupo, Guanarito, and Sabia).
In response to the West Africa EVD epidemic, enhanced screening of all airline passengers who had traveled to Liberia, Sierra Leone, and Guinea within the previous 21 days continued into 2015; enhanced screening was progressively discontinued as control measures brought the epidemic to a close in these countries. Entry risk assessment and active monitoring was discontinued for travelers returning from Liberia in September and from Sierra Leone in December. Over the duration of the enhanced entry risk assessment and management program, approximately 38,000 travelers were assessed at U.S. ports of entry (2).
In May 2015, a returning traveler from Liberia presented to a New Jersey hospital with illness that was laboratory-confirmed to be Lassa fever. This patient later died. This is the eighth known imported case to the United States (3). Lassa fever is endemic in West Africa, with an estimated 100,000 to 300,000 cases and 5,000 deaths annually. Physicians should remain aware of the potential for VHF infections in recent travelers.
- Rollin PE, Nichol ST, Zaki S, Ksiazek TG. Arenaviruses and filoviruses. In: Murray PR, Baron EJ, Landry ML, Jorgensen JH, Pfaller MA, eds. Manual of clinical microbiology, 11th ed. Washington, DC: ASM Press; 2015:1669–86.
- Cohen NJ, Brown CM, Alvarado-Ramy F, et al. Travel and border health measures to prevent the international spread of Ebola. MMWR Suppl 2016;65(No. Suppl 3);57–67.
- Amorosa V, MacNeil A, McConnell R, et al. Imported Lassa fever, Pennsylvania, USA, 2010. Emerg Infect Dis 2010;16:1598–600. CrossRefexternal icon PubMedexternal icon
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), (ArboNET Surveillance), as of July 1, 2016.
§ Totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
¶ Reportable in <25 states.
** Total number of cases reported from 42 states. Reports might not reflect unique cases.
†† Total number of cases reported from 42 states.
§§ Total number of cases reported from 39 states. Reports might not reflect unique cases.
¶¶ Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2016.
*** Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases (NCIRD), as of June 30, 2016
††† Totals reported to the Division of High-Consequence Pathogens and Pathology, NCEZID (National Rabies Surveillance System), as of December 31, 2016.
§§§ Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
¶¶¶ Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
**** Totals reported to the Division of Viral Diseases, NCIRD, as of June 30, 2016.
C.N.M.I.: Commonwealth of Northern Mariana Islands
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
†Totals reported to the Division of Vector-Borne Diseases (DVBD), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) (ArboNET Surveillance), as of July 1, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases (DVBD), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) (ArboNET Surveillance), as of July 1, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
†Includes cases reported as wound and unspecified botulism.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of STD Prevention (DSTDP), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
§ Notifiable in <25 states.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Total number of reported laboratory-positive dengue cases including all confirmed cases [by anti-dengue virus (DENV) molecular diagnostic methods or seroconversion of anti-DENV IgM] and all probable cases (by a single, positive anti-DENV IgM). Totals reported to the Division of Vector-Borne Diseases (DVBD), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) (ArboNET Surveillance), as of July 1, 2016.
* No cases of anthrax; Crimean-Congo hemorrhagic fever; dengue hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola hemorrhagic fever; Guanarito hemorrhagic fever; Junin hemorrhagic fever; Lujo virus; Machupo hemorrhagic fever; Marburg fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia-associated hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease (SARS-CoV); smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of STD Prevention (DSTDP), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals number of cases reported from 42 states. Reports might not reflect unique cases.
§ Total number of cases reported from 42 states.
¶ Total number of cases reported from 39 states. Reports might not reflect unique cases.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
†Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2015.
§Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases (NCIRD), as of June 30, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of High-Consequence Pathogens and Pathology (DHCPP), National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) (ArboNET Surveillance), as of December 31, 2015.
§ Includes Escherichia coli O157:H7; shiga toxin-positive, serogroup non-O157; and shiga toxin positive, not serogrouped.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Since January 1, 2010, “Invasive pneumococcal disease (IPD)” has been nationally notifiable and separate notifications for “Drug-resistant S. pneumoniae” and “IPD in children <5 years of age” have been discontinued.
§ Invasive pneumococcal disease.
¶ Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
*** Totals reported to the Division of STD Prevention (DSTDP), National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
†Totals reported to the Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, as of June 8, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
†Totals reported to the Division of Viral Diseases (DVD), National Center for Immunization and Respiratory Diseases (NCIRD), as of May 2, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fevers; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Month is defined using MMWR week (https://wwwn.cdc.gov/nndss/document/MMWR_Week_overview.pdfpdf icon). MMWR week calendars can be found at https://wwwn.cdc.gov/nndss/script/downloads.aspx.
§ Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) (ArboNET Surveillance), as of July 1, 2016.
¶Totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
** Reportable in <25 states.
†† Total number of cases reported from 42 states. Reports might not reflect unique cases.
§§ Total number of cases reported from 42 states.
¶¶ Total number of cases reported from 39 states. Reports might not reflect unique cases.
*** Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2016.
††† Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases (NCIRD), as of June 30, 2016.
§§§ Totals reported to the Division of High-Consequence Pathogens and Pathology, NCEZID (National Rabies Surveillance System), as of December 31, 2016.
¶¶¶ Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
**** Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
†††† Totals reported to the Division of Viral Diseases, NCIRD, as of June 30, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance), as of July 1, 2016.
§ Cases among persons aged <15 years are not shown (except for Syphilis, congenital); totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
¶ Data are suppressed for those aged <15 years. The count displayed in the “Total” column reflects the total count across all age groups for this condition.
** Reportable in <25 states.
†† Total number of cases reported from 42 states. Reports might not reflect unique cases.
§§ Total number of cases reported from 42 states.
¶¶ Total number of cases reported from 39 states. Reports might not reflect unique cases.
*** Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2016.
††† Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases, as of June 30, 2016.
§§§ Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis. Totals reported to the DSTDP, NCHHSTP, as of June 8, 2016.
¶¶¶ Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
* No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance), as of July 1, 2016.
§ Totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
¶ Reportable in <25 states.
** Total number of cases reported from 42 states. Reports might not reflect unique cases.
†† Total number of cases reported from 42 states.
§§ Total number of cases reported from 39 states. Reports might not reflect unique cases.
¶¶ Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2016.
***Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases, as of June 30, 2016.
††† Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
§§§ Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
* Conditions for which <25 cases were reported for the year are not included in the table. No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance), as of July 1, 2016.
§ Totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
¶ Reportable in <25 states.
** Total number of cases reported from 42 states. Reports might not reflect unique cases.
†† Total number of cases reported from 42 states.
§§ Total number of cases reported from 39 states. Reports might not reflect unique cases.
¶¶ Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31, 2016.
*** Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases, as of June 30, 2016.
††† Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
§§§ Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
* Conditions for which <25 cases were reported for the year are not included in the table. No cases of anthrax; Crimean-Congo viral hemorrhagic fever; diphtheria; eastern equine encephalitis virus disease, nonneuroinvasive; Ebola viral hemorrhagic fever; Guanarito viral hemorrhagic fever; Junin viral hemorrhagic fever; Lujo viral hemorrhagic fever; Machupo viral hemorrhagic fever; Marburg viral hemorrhagic fever; poliomyelitis, paralytic; poliovirus infection, nonparalytic; Sabia viral hemorrhagic fever; severe acute respiratory syndrome-associated coronavirus disease; smallpox; western equine encephalitis virus disease, neuroinvasive and nonneuroinvasive; and yellow fever were reported in the United States during 2015.
† Totals reported to the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance), as of July 1, 2016.
§ Totals reported to the Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP), as of June 8, 2016.
¶ Reportable in <25 states.
**Total number of cases reported from 42 states. Reports might not reflect unique cases.
††Total number of cases reported from 42 states.
§§Total number of cases reported from 39 states. Reports might not reflect unique cases
¶¶Total number of HIV diagnoses reported to the Division of HIV/AIDS Prevention, NCHHSTP through December 31,
2016.
*** Totals reported to the Influenza Division, National Center for Immunization and Respiratory Diseases, as of June 30, 2016.
††† Includes the following categories: primary, secondary, early latent, late latent, late with clinical manifestations, and congenital syphilis.
§§§ Totals reported to the Division of Tuberculosis Elimination, NCHHSTP, as of June 8, 2016.
| U | Data not available. |
| N | Not reportable (i.e., report of disease not required in that jurisdiction). |
| DC | District of Columbia |
| NYC | New York City |
| AS | American Samoa |
| CNMI | Commonwealth of Northern Mariana Islands |
| GU | Guam |
| PR | Puerto Rico |
| VI | U.S. Virgin Islands |
ANTHRAX. Number of reported cases, by year — United States, 1960–2015*
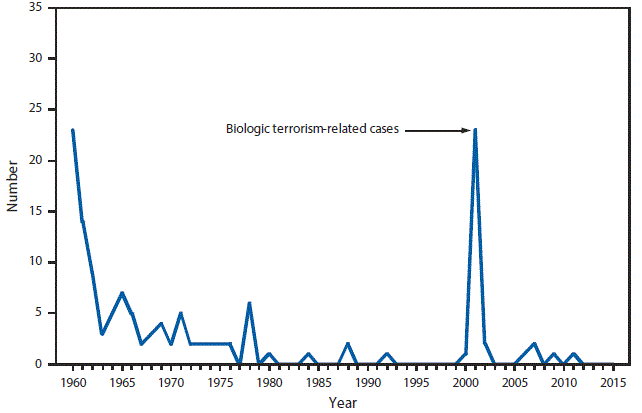
* One epizootic-associated cutaneous case was reported in 2001 from Texas.
In 2015, there were no reported human anthrax cases from zoonotic or other causes.
ARBOVIRAL DISEASES. Number* of reported cases of selected neuroinvasive disease, by year — United States, 2006–2015
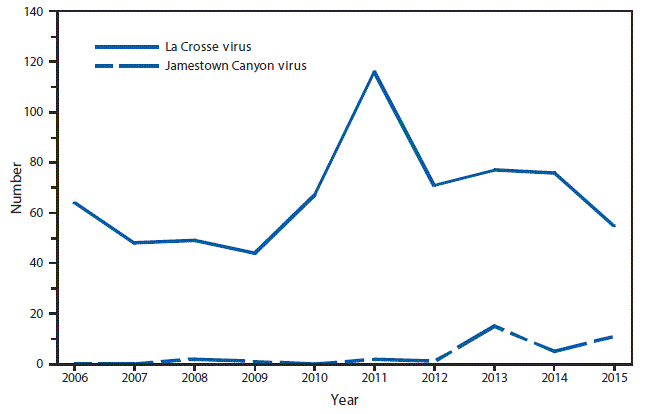
* Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance). Only reported cases of neuroinvasive disease are shown.
During 2006–2015, an average of 66 La Crosse virus neuroinvasive disease cases were reported each year. La Crosse virus was the most common cause of neuroinvasive arboviral disease among children. During that same time period, Jamestown Canyon virus caused an average of three neuroinvasive disease cases per year. Starting in 2013, following the implementation of routine antibody testing for Jamestown Canyon virus disease, the number of reported cases has increased.
ARBOVIRAL DISEASES, CHIKUNGUNYA VIRUS. Number of reported cases, by year,* excluding U.S. territories — United States, 2010–2015
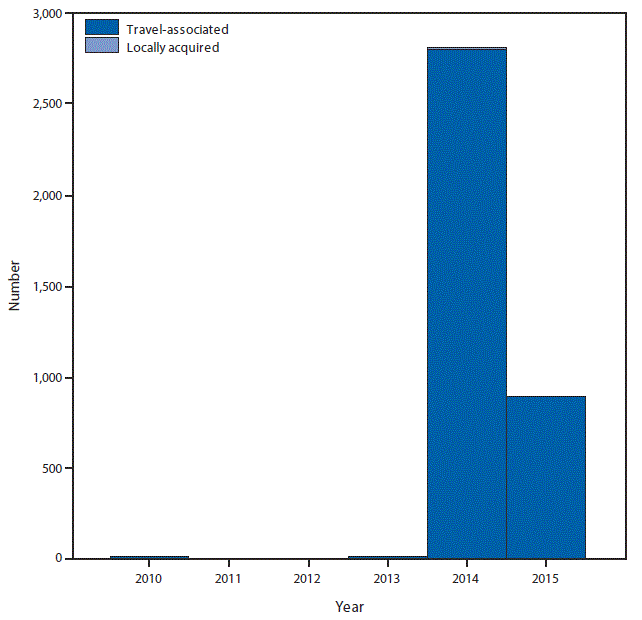
* Chikungunya virus did not become a nationally notifiable condition until 2015.
In 2015, a total of 896 chikungunya virus disease cases were reported. One locally acquired case was reported from Texas. All other cases occurred in travelers returning from affected areas.
ARBOVIRAL DISEASES, WEST NILE VIRUS. Incidence* of reported cases of neuroinvasive disease, by age group—United States, 2015
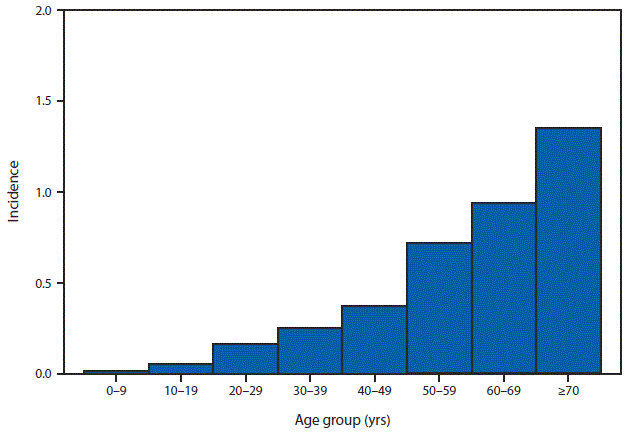
* Per 100,000 population. Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance).
In 2015, West Nile virus neuroinvasive disease incidence increased with increasing age, from 0.04 per 100,000 among persons aged <18 years to 1.36 among those aged ≥70 years.
ARBOVIRAL DISEASES, WEST NILE VIRUS. Incidence* of reported cases of neuroinvasive disease—United States and U.S. territories, 2015
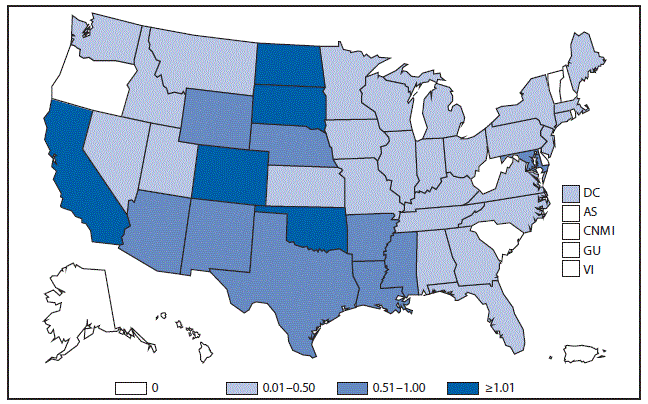
* Per 100,000 population. Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance).
In 2015, the states with the highest reported incidence of West Nile virus (WNV) neuroinvasive disease were California (1.49 per 100,000), North Dakota (1.32), South Dakota (1.28), Oklahoma (1.25) and Colorado (1.04). Over half (61%) of all WNV neuroinvasive disease cases were reported from California (585 cases) and Texas (196).
ARBOVIRAL DISEASES, WEST NILE VIRUS. Incidence* of reported cases of neuroinvasive disease, by year—United States, 2006–2015
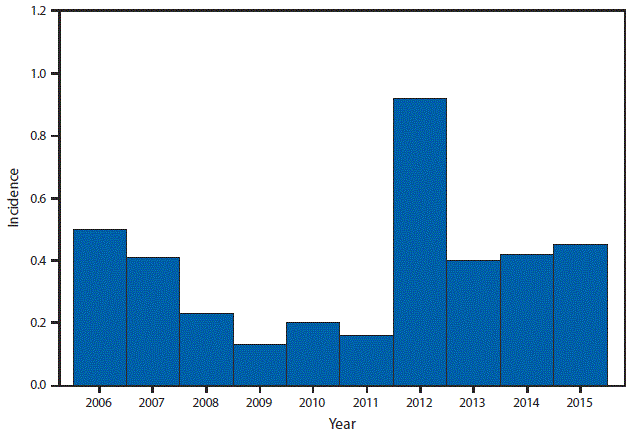
* Per 100,000 population. Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance).
Nationally, West Nile virus neuroinvasive disease incidence in 2015 was similar to the median incidence during 2006–2014.
BABESIOSIS. Number of reported cases, by county — United States, 2015
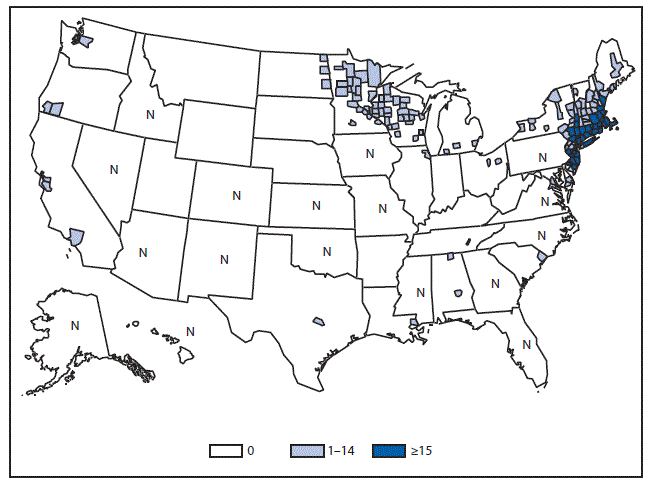
Abbreviation: N = not reportable.
In 2015, babesiosis was reportable in 33 states. Twenty-four of the 33 states notified CDC of at least one case of babesiosis; however, 93% of the reported cases (n = 1,925/2,074) occurred in residents of seven of the states in which tickborne transmission of Babesia microti has been well documented (i.e., in Connecticut, Massachusetts, New Jersey, New York, and Rhode Island in the Northeast; and Minnesota and Wisconsin in the upper Midwest).
BOTULISM, FOODBORNE. Number of reported cases, by year — United States, 1995–2015
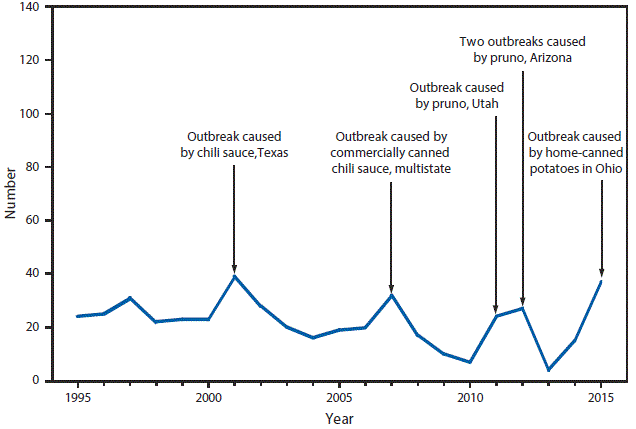
In 2015, most of the foodborne botulism cases, caused by ingestion of food containing preformed toxin, occurred in an outbreak associated with home-canned potatoes in a potato salad consumed at a church potluck. Pruno, which caused the 2011 and 2012 outbreaks in Utah and Arizona, respectively, is an illicit alcoholic beverage brewed by prison inmates.
BOTULISM, INFANT. Number of reported cases, by year — United States, 1995–2015
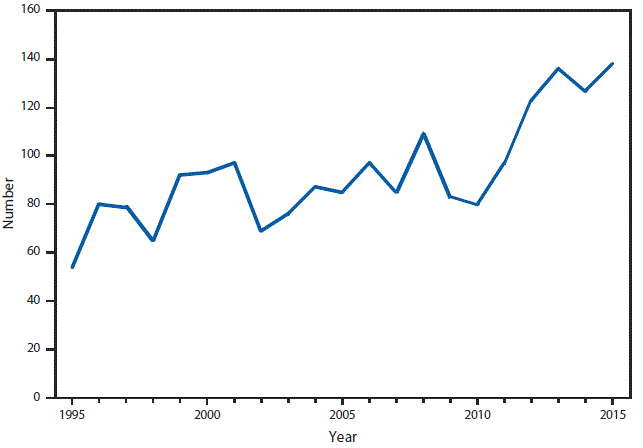
Infant botulism remains the most common type of botulism in the United States and accounted for most botulism cases in 2015. Reported cases have increased overall since 2010.
BOTULISM, OTHER. Number of reported cases, by year — United States, 2005–2015
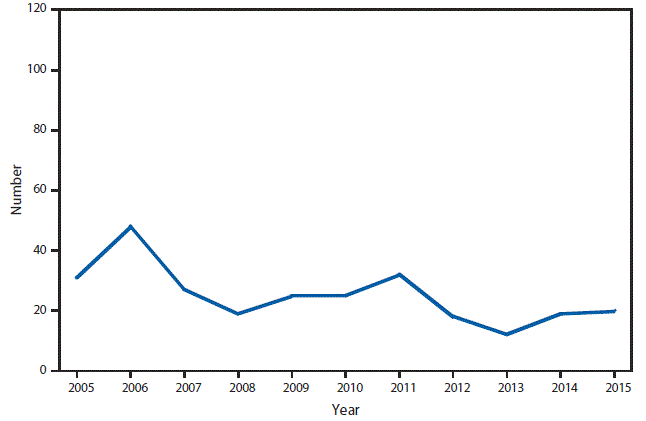
Annual number of cases of wound botulism and of botulism in “unspecified” transmission categories have remained generally unchanged since 2007.
BRUCELLOSIS. Number of reported cases — United States and U.S. territories, 2015
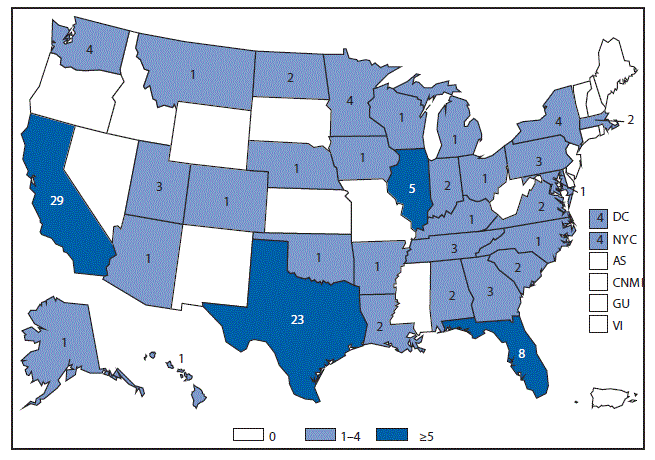
Cases in Illinois, Florida, Texas, and California combined represent over half of the brucellosis cases reported to NNDSS during 2015 (65/126; 52%).
BRUCELLOSIS. Number of reported cases, by year — United States, 1985–2015
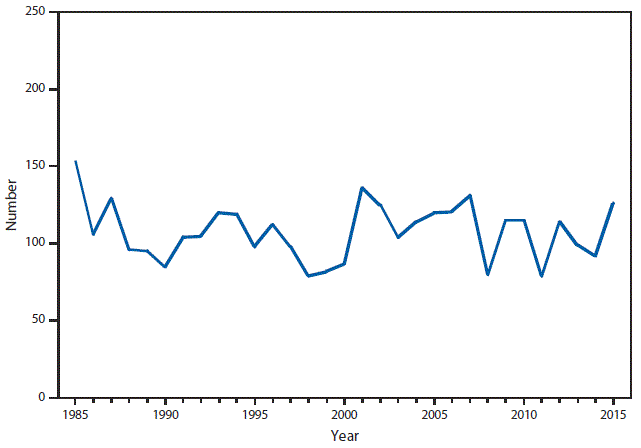
The number of brucellosis cases reported to NNDSS has fluctuated since 1985, showing no particular trend.
CAMPYLOBACTERIOSIS. Incidence* of reported cases — United States and U.S. territories, 2015
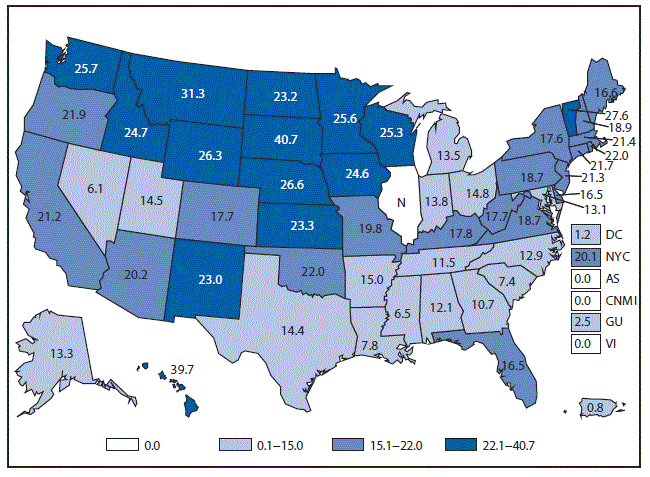
Abbreviation: N = not reportable.
* Per 100,000 population.
Incidence of confirmed and probable campylobacteriosis was highest in northern and western states.
CHLAMYDIA. Incidence* of reported cases among women aged 15–24 years — United States and U.S. territories, 2015
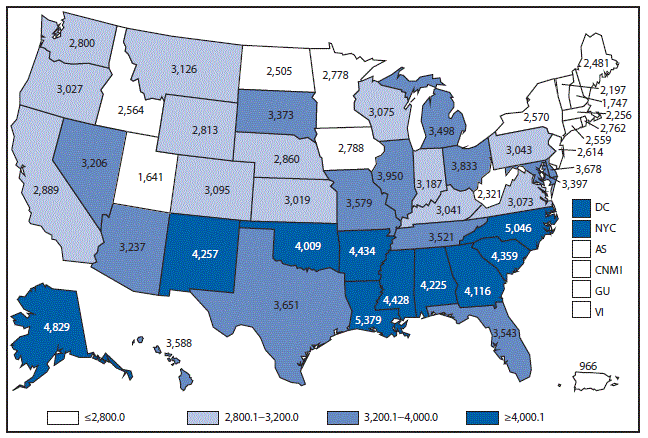
* Per 100,000 population. Rate of reported cases for DC (5,974), New York City (4,296), Guam (466), and Virgin Island (1,009). Rates for AS and CNMI are not available.
The overall rate of reported cases of chlamydia among women aged 15–24 years, which is the population targeted for chlamydia screening, was 3,377.6 per 100,000 females (excluding U.S. territories). There was variation by state, with the Southern region reporting the highest case rates.
CHLAMYDIA. Incidence* of reported cases, by age group and sex — United States, 2015
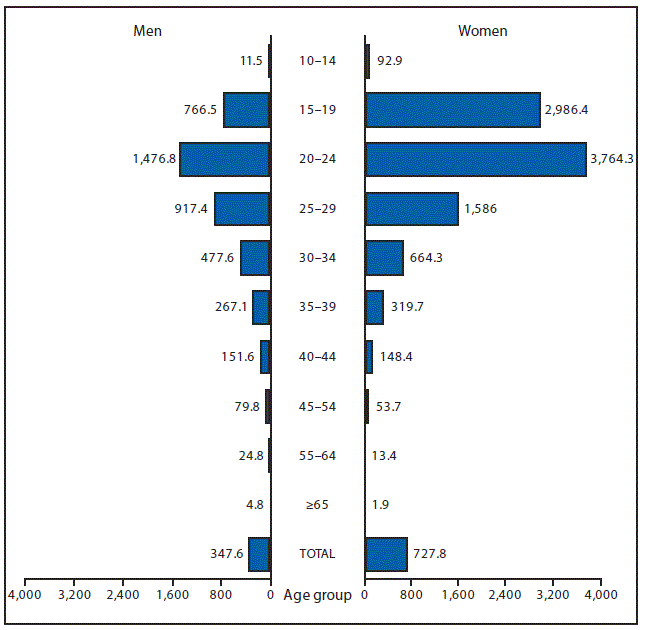
* Per 100,000 population.
The highest age-specific rates of reported cases of chlamydia among women in 2015 were in those aged 20–24 years (3,764.3 cases per 100,000 females) followed by those aged 15–19 years (2,986.4 cases per 100,000 females). The age-specific rates of reported cases of chlamydia among men, despite being consistently about half the rate of women, were similarly highest in men aged 20–24 years (1,476.8 cases per 100,000 males) followed by men aged 15–19 years (766.5 cases per 100,000 males).
CHOLERA. Number of reported cases — United States and U.S. territories, 2015
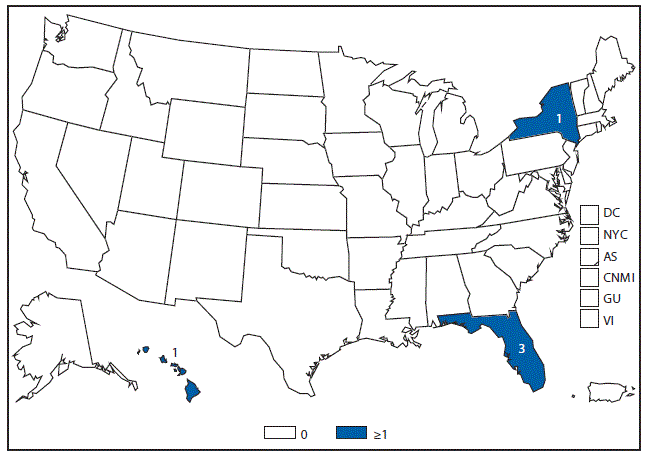
In 2015, five cases of cholera were reported from three states. Four cases were travel-associated, and one case was associated with the consumption of imported seafood.
COCCIDIOIDOMYCOSIS. Number of reported cases — United States and U.S. territories, 2015
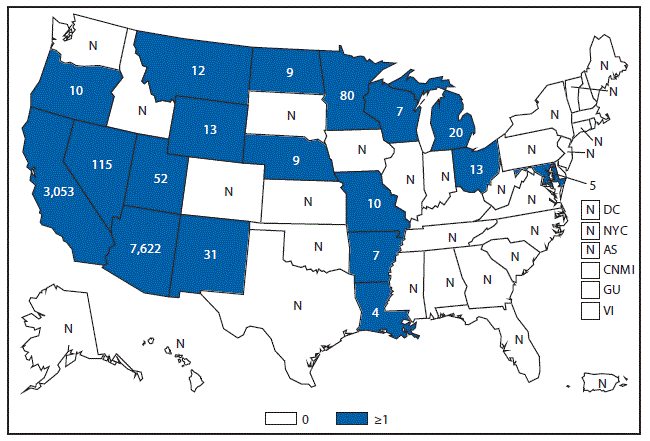
Abbreviation: N = not reportable.
In the United States, coccidioidomycosis is endemic in the Southwestern states. The fungus that causes coccidioidomycosis has also been found in south-central Washington State. Cases reported from states outside the endemic area usually occur among travelers returning from areas in which the disease is endemic.
CRYPTOSPORIDIOSIS. Incidence* of reported cases, by year — United States, 2004–2015
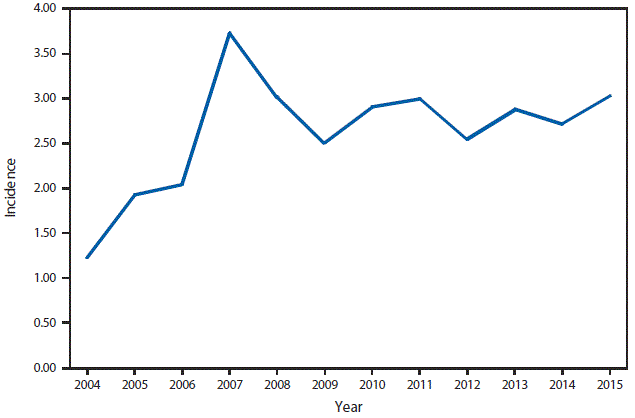
* Per 100,000 population.
The incidence of reported cryptosporidiosis after 2007 remains elevated (>2.5 cases per 100,000 population) relative to the baseline observed before 2005 (<1.5). Whether this increase reflects a change in the true incidence of cryptosporidiosis or changing diagnosis, testing, or reporting patterns is unclear.
CRYPTOSPORIDIOSIS. Incidence* of reported cases — United States and U.S. territories, 2015
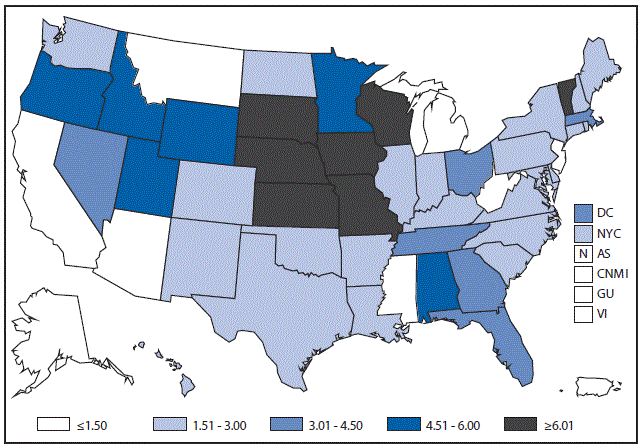
Abbreviation: N = not reportable.
* Per 100,000 population.
Cryptosporidiosis is widespread geographically in the United States. Although incidence appears to be consistently higher in certain states, differences in incidence among states might reflect differences in risk factors; the number of cases associated with outbreaks; or the capacity to detect, investigate, and report cases.
CYCLOSPORIASIS. Number of reported cases — United States and U.S. territories, 2015
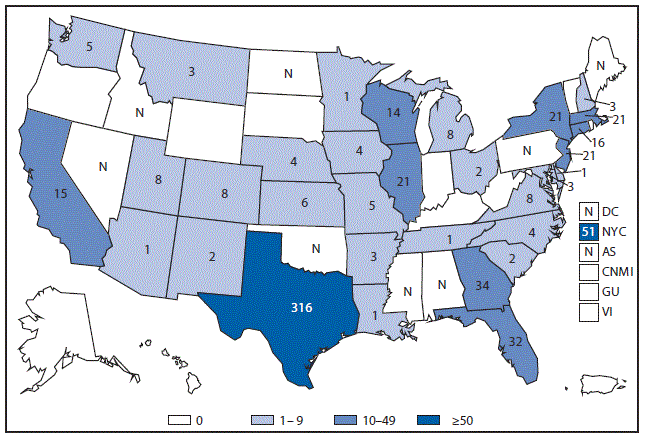
Abbreviation: N = not reportable.
In 2015, a total of 644 cyclosporiasis cases (599 confirmed and 45 probable) were reported from 32 states and New York City. This number differs slightly from the denominator of 645 cases reported in the tables. One erroneous report was not retracted before the deadline for finalizing the data. Of the 644 cases, 394 (61%) were domestically acquired (i.e., they occurred in persons with no history of travel outside the United States and Canada during the 14-day incubation period), at least 357 (91%) of which occurred in persons with illness onset during May–August. A vehicle of infection (fresh cilantro from Mexico) was identified for 61 restaurant-associated cases in a multistate outbreak involving Georgia, Texas, and Wisconsin. An additional 29 probable cases were associated with this multicluster outbreak but were not reported to NNDSS or included here.
DENGUE. Number* of reported cases, by age group — United States, 2015
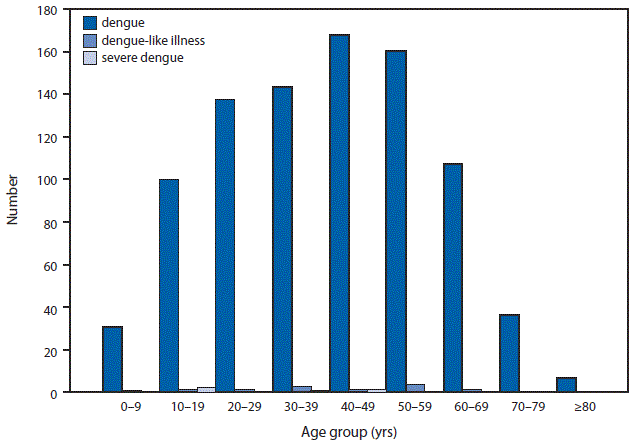
* Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance). Two age-unknown cases of dengue. No age-unknown cases of dengue-like illness and severe dengue.
In 2015, a total of 929 dengue cases were reported in all age groups, but most (77%) cases were among adults aged 18–64 years. Sixteen cases of dengue-like illness were reported, 14 (88%) of which were in adults aged 18–64 years. Six cases of severe dengue were reported in patients aged 12–48 years.
DENGUE. Number* of reported cases, by location of residence — United States and U.S. territories, 2015
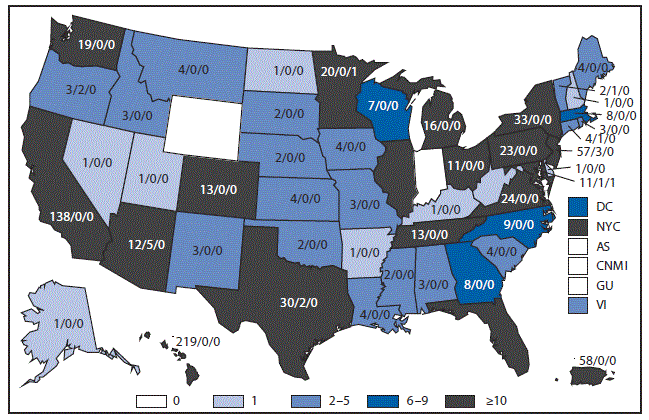
* Number of dengue/dengue-like illness/severe dengue cases. Data from the Division of Vector-Borne Diseases, National Center for Emerging and Zoonotic Infectious Diseases (ArboNET Surveillance). The reported cases for DC (8/2/1), NYC (74/1/1), and VI (3/0/0).
In 2015, a total of 951 laboratory-positive dengue cases were reported from 48 of the 50 states, two of the five territories, and the District of Columbia. Sixteen cases of dengue-like illness and six cases of severe dengue were reported, all in travelers and none in residents of U.S. territories. The states that reported the most travel-associated cases of dengue, dengue-like illness, or severe dengue were California (138), Florida (81), New York City (76), New Jersey (60), and Texas (32). States that reported locally acquired dengue cases were Hawaii (200) and Florida (1).
DIPHTHERIA. Number of reported cases, by year — United States, 1985–2015
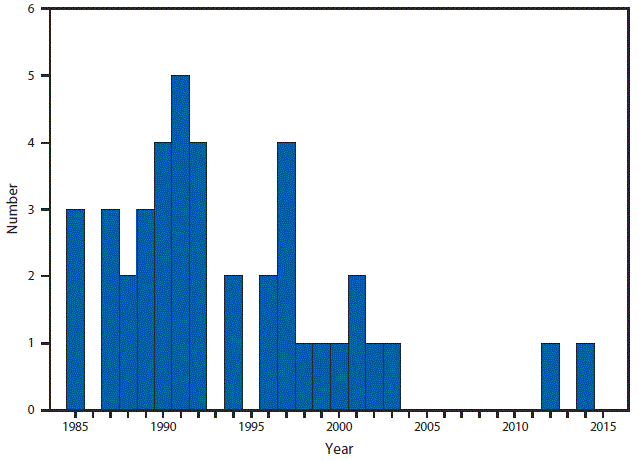
Diphtheria is rare in the United States. No cases were reported during 2015.
EHRLICHIOSIS AND ANAPLASMOSIS, ANAPLASMA PHAGOCYTOPHILUM. Number of reported cases, by county — United States, 2015
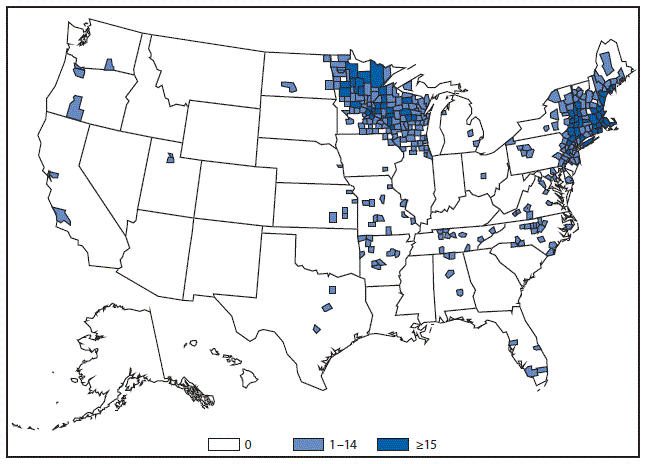
Anaplasma phagocytophilum is primarily transmitted by Ixodes scapularis in the eastern United States and Ixodes pacificus in the west. Minnesota, Wisconsin, New York and Massachusetts continue to report the highest number of anaplasmosis cases.
EHRLICHIOSIS AND ANAPLASMOSIS, EHRLICHIA CHAFFEENSIS. Number of reported cases, by county — United States, 2015
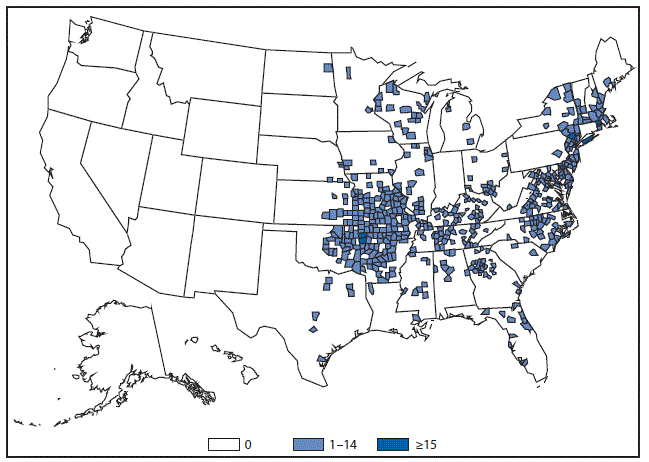
Ehrlichia chaffeensis is the most common cause of human ehrlichiosis in the United States. Cases are primarily distributed within the central United States within the known distribution of the principle vector, Amblyomma americanum.
EHRLICHIOSIS AND ANAPLASMOSIS, EHRLICHIA EWINGII. Number of reported cases, by county — United States, 2015
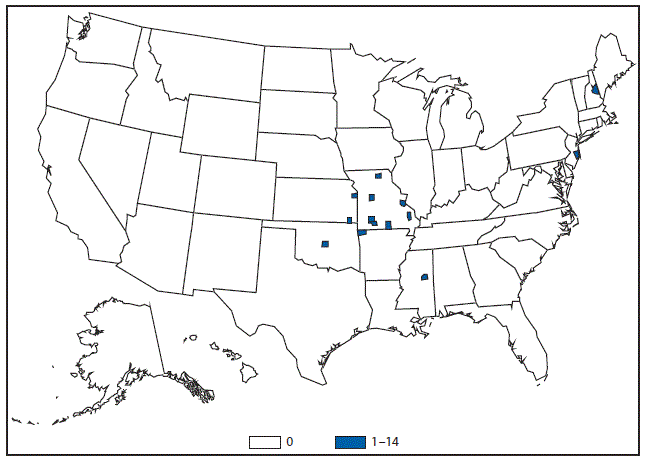
Ehrlichia ewingii is a less commonly reported cause of human ehrlichiosis. Cases of Ehrlichia ewingii are primarily reported from the Midwest and have recently expanded to include regions such as the Northeast.
EHRLICHIOSIS AND ANAPLASMOSIS, UNDERTERMINED. Number of reported cases, by county — United States, 2015
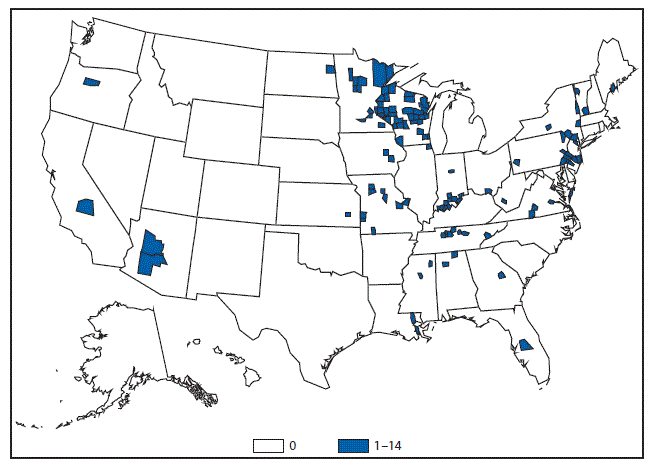
The reporting category of undetermined ehrlichiosis/anaplasmosis is used in situations where multiple Ehrlichia or Anaplasma species might be present yet laboratory evidence is unable to provide species differentiation. Cases in this category are reported throughout the United States.
GIARDIASIS. Incidence* of reported cases, by year — United States, 2004–2015
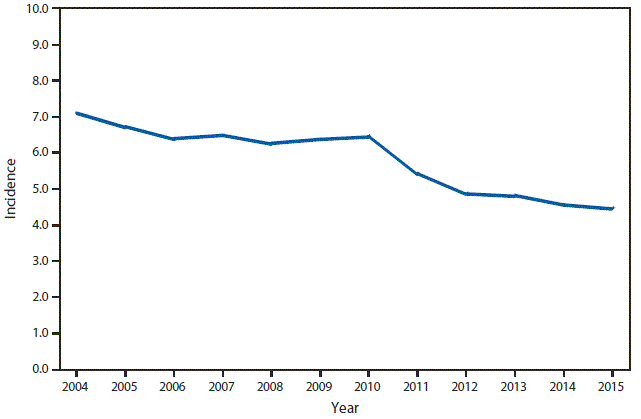
* Per 100,000 population
The incidence of giardiasis in 2015 is similar to previous years, following a decline in 2011. The incidence of giardiasis can be affected by actual changes in disease transmission, changes in diagnostics, and changes in surveillance priorities in some states.
HAEMOPHILUS INFLUENZAE, INVASIVE DISEASE. Incidence* of reported cases among persons aged <5 years, by serotype — United States, 2002–2015
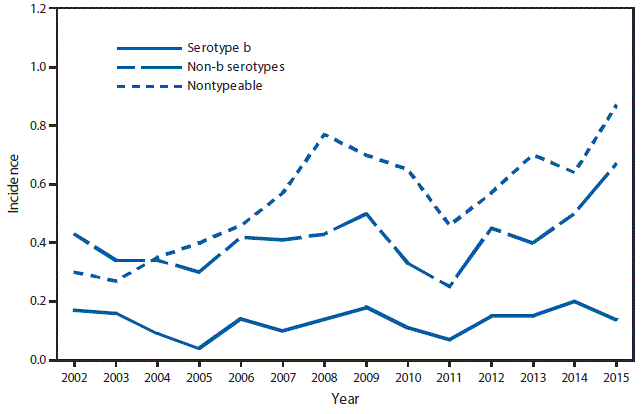
* Per 100,000 population. Cases for which serotype was not tested or is unknown are excluded.
Rates of all invasive Haemophilus influenza disease remain low; the majority of cases of invasive disease in children aged <5 years are caused by nontypeable Haemophilus influenzae. Haemophilus influenza type b incidence remains below the Healthy People 2020 goal of 0.27 per 100,000 population among those aged <5 years.
HAEMOPHILUS INFLUENZAE, INVASIVE DISEASE. Incidence* of reported cases among persons aged ≥5 years, by serotype — United States, 2002–2015

* Per 100,000 population. Cases for which serotype was not tested or is unknown are excluded.
Rates of all invasive Haemophilus influenzae disease remain low; the majority of cases of invasive disease in persons aged ≥5 years are caused by nontypeable Haemophilus influenzae.
HANSEN’S DISEASE (LEPROSY). Number of reported cases, by year — United States, 1995–2015
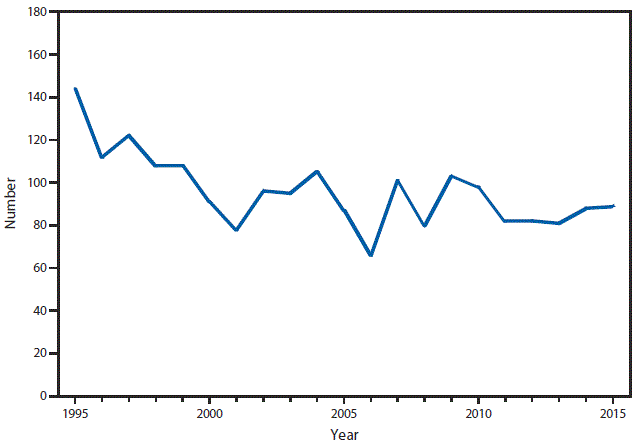
After a decrease in reported Hansen’s disease cases during 2010–2011, the number of reported cases has remained fairly stable. In the last decade, the highest number of Hansen’s disease cases reported was in 2009. Reported cases for 2014 and 2015 remained stable.
HEMOLYTIC UREMIC SYNDROME, POSTDIARRHEAL. Number of reported cases — United States and U.S. territories, 2015
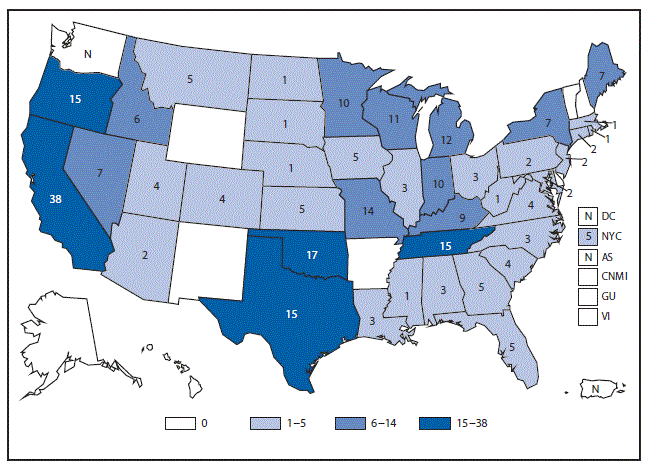
Abbreviation: N = not reportable.
In 2015, a total of 42 of 56 jurisdictions (states, districts, and territories) reported hemolytic uremic syndrome (HUS) cases to NNDSS, and four jurisdictions had missing data. Most cases of postdiarrheal HUS are caused by Shiga toxin-producing Escherichia coli (STEC).
HUMAN IMMUNODEFICIENCY VIRUS DIAGNOSES. Percentage of diagnosed cases, by race/ethnicity — United States, 2015
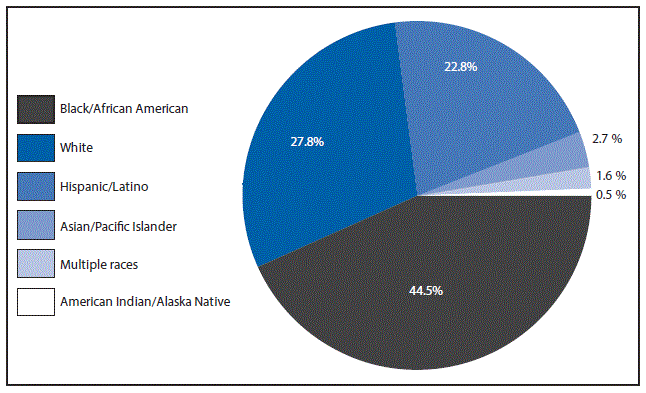
Among persons with HIV infection diagnosed in 2015, the greatest percentage was among blacks/African Americans, followed by whites, Hispanics/Latinos, Asians/Pacific Islanders, persons of multiple races, and American Indians/Alaska Natives.
HUMAN IMMUNODEFICIENCY VIRUS DIAGNOSES. Diagnosis incidence* — United States and U.S. territories, 2015
* Per 100,000 population.
The highest rates (i.e., ≥15 diagnoses per 100,000 population) of HIV diagnoses were in certain states in the Southeast and Northeast. A rate of ≥15 diagnoses per 100,000 population also was observed in the District of Columbia.
INFLUENZA-ASSOCIATED PEDIATRIC MORTALITY. Incidence* of reported cases — United States and U.S. territories, 2015
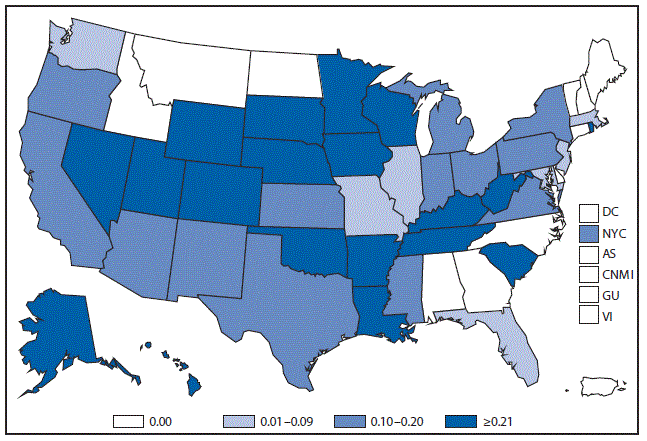
* Per 100,000 population.
In 2015, New York City and 39 states reported 130 influenza-associated pediatric deaths for an overall incidence rate of 0.18 deaths per 100,000 children aged <18 years.
LEGIONELLOSIS. Incidence* of reported cases, by year — United States, 2000–2015
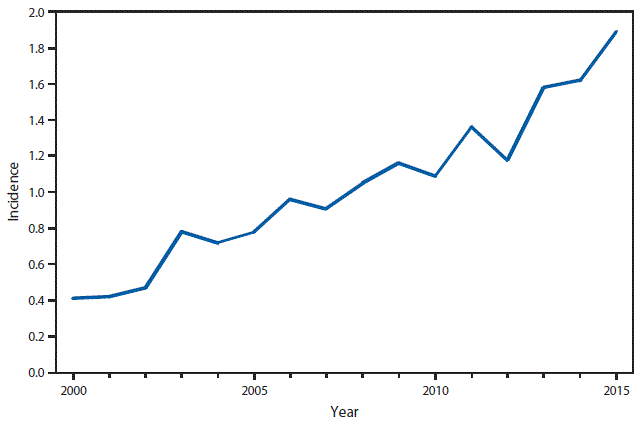
* Per 100,000 population.
From 2014 to 2015, the reported incidence of Legionellosis rose over 16%, continuing an upward trend that began in 2003. The incidence in 2015 was more than four times that in 2000. More diagnostic testing and more disease transmission might have contributed to this increase.
LEPTOSPIROSIS. Number of reported cases, by year — United States and U.S. territories, 1947–2015
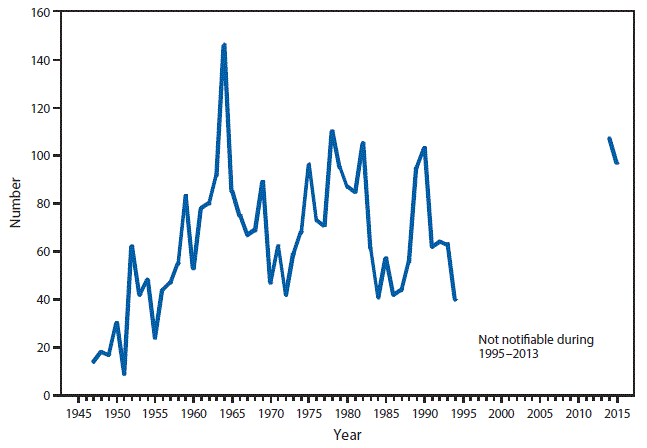
In 2015, a total of 96 leptospirosis cases were reported, of which 45 (47%) were reported by Puerto Rico and 22 (23%) were reported by Hawaii. A temporal peak in case incidence occurred in August, with 10 cases reported that month in five states and jurisdictions (excluding cases reported from territories).
Note: Although leptospirosis was first notifiable starting in 1947, territories did not begin reporting leptospirosis cases until 1959. Territory data for 1970 and 1978 are not available.
LISTERIOSIS. Incidence* of reported cases — United States and U.S. territories, 2015
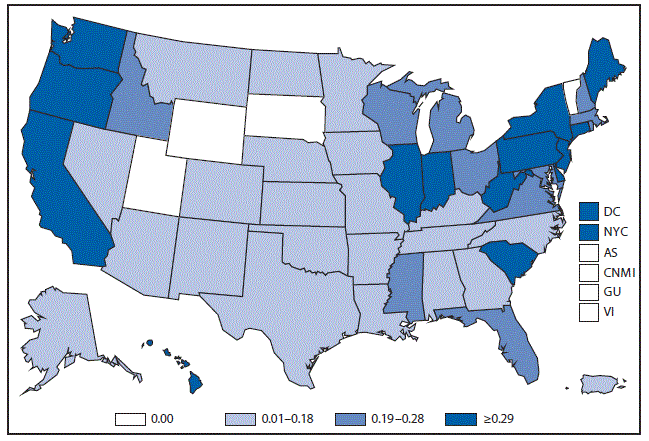
* Per 100,000 population.
In 2015, a total of 46 states, the District of Columbia, and New York City reported 768 cases of Listeriosis to NNDSS for an overall incidence rate in the United States of 0.24 infections per 100,000, which is unchanged from 2014.
LYME DISEASE. Incidence* of reported confirmed cases, by county — United States, 2015
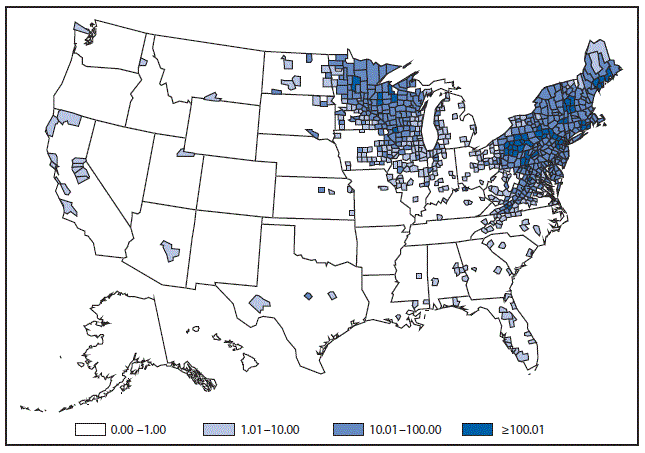
* Per 100,000 population.
Lyme disease was the most commonly reported vector-borne disease in 2015; however, risk for infection is highly variable, with little to no risk in many parts of the United States. Cases are concentrated in the northeast and upper Midwest regions of the United States. In 2015, 95% of confirmed Lyme disease cases were reported from 14 states: Connecticut (1,873 cases), Delaware (334 cases), Maine (993 cases), Maryland (1,249 cases), Massachusetts (2,922 cases), Minnesota (1,174 cases), New Hampshire (436 cases), New Jersey (3,932 cases), New York (3,252 cases), Pennsylvania (7,351 cases), Rhode Island (564 cases), Vermont (491 cases), Virginia (1,102 cases), and Wisconsin (1,309 cases). Lyme disease cases are reported to CDC by state of patient residence; therefore, travel-associated cases might be reported from states where risk for infection is absent.
MEASLES. Incidence* of reported cases by year — United States, 1980–2015
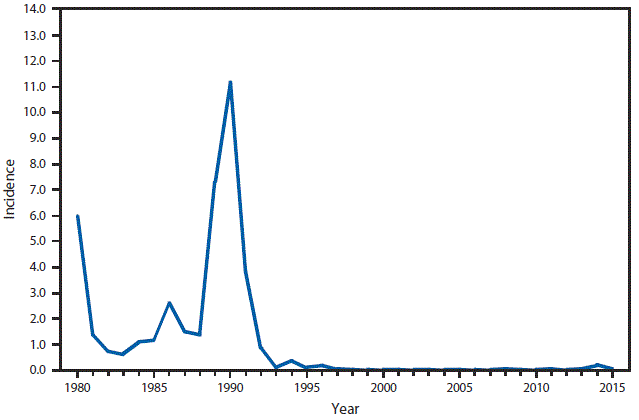
* Per 100,000 population.
Although measles incidence rates declined substantially soon after licensure of a measles vaccine in the United States in 1963, outbreaks continued to be reported across the country through the 1980s, and a resurgence of measles occurred during 1989–1991. Improvements in vaccination coverage in the early and mid-1990s led to a record low number of cases in ensuing years, and a declaration of measles elimination in 2000. Since 1997, the reported annual incidence has been <1 case per 1 million population, except in 2014, when measles was introduced into several communities with pockets of unvaccinated persons, which allowed spread and outbreaks to occur.
MENINGOCOCCAL DISEASE. Incidence* of reported cases, by year — United States, 1985–2015
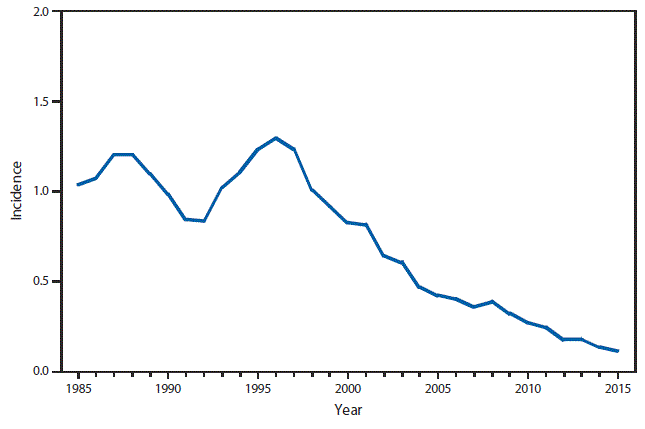
* Per 100,000 population.
In 2015, meningococcal disease incidence continued to decline; incidence remains at a historic low in the United States (0.12 cases per 100,000 population.
MUMPS. Incidence* of reported cases, by year — United States, 1990–2015
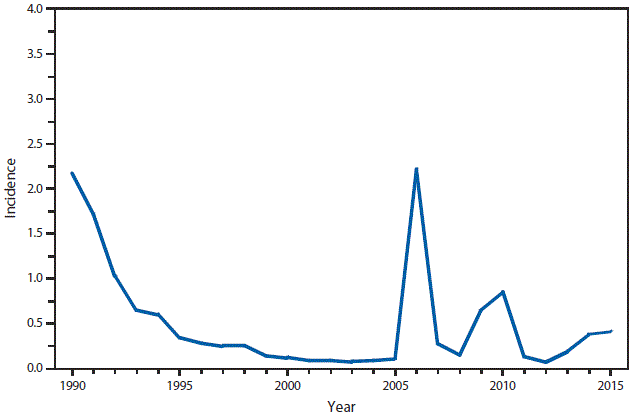
* Per 100,000 population.
The widespread use of a second dose of mumps vaccine beginning in 1989 was followed by historically low morbidity until 2006, when the United States experienced the largest mumps outbreak in two decades. The 2006 outbreak of approximately 6,000 cases primarily affected college students in the Midwest. A second large outbreak occurred during 2009–2010 and affected Orthodox Jewish communities in the Northeast. Multiple outbreaks have occurred in the following years, mostly in close-contact settings.
PERTUSSIS. Incidence* of reported cases, by age — United States, 2015
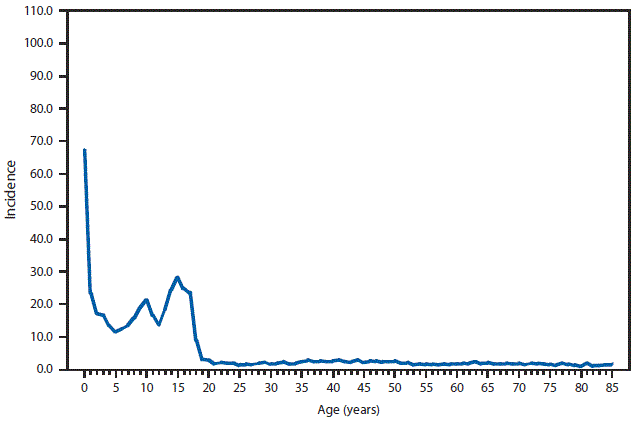
* Per 100,000 population.
During 2015, pertussis incidence remained highest among infants, and increased incidence continues to be observed among adolescents.
PERTUSSIS. Incidence* of reported cases, by year — United States, 1985–2015
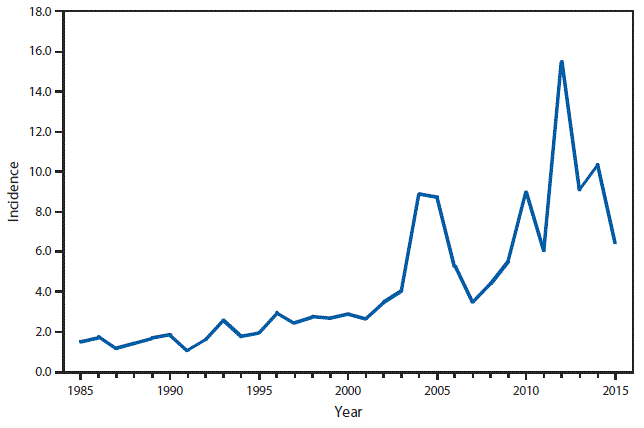
* Per 100,000 population.
Incidence of reported pertussis declined from 2014 to 2015; however, overall incidence remains elevated compared with rates observed during the 1990s and early 2000s.
RABIES, ANIMAL. Number* of reported cases, by county — United States, 2015
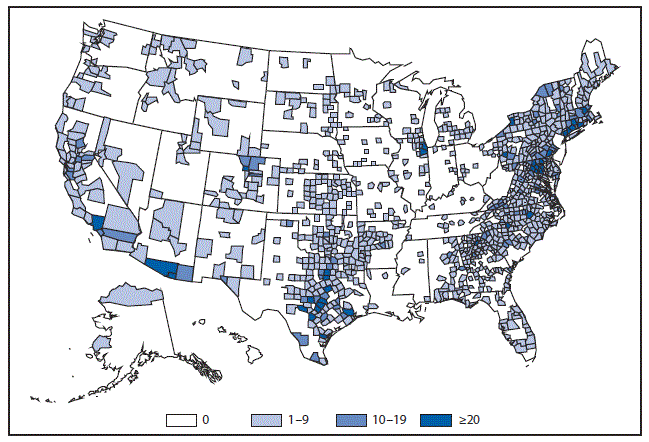
* Data from the Division of High Consequence Pathogens and Pathology, National Center for Emerging and Zoonotic Infectious Diseases.
In 2015, rabid animals were reported in all jurisdictions except Hawaii. Because reporting is based on the number of animals tested, the burden of disease is likely underestimated.
SALMONELLOSIS AND SHIGELLOSIS. Incidence* of reported cases, by year — United States, 1985–2015
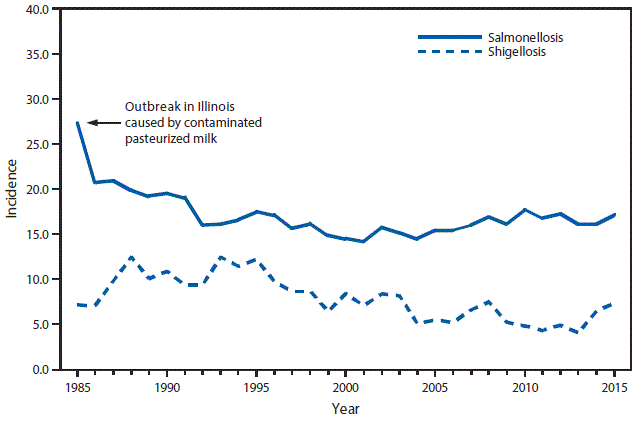
* Per 100,000 population.
Incidence of salmonellosis has been stable since the mid-1990s. Incidence of shigellosis decreased overall between 1995 and 2013 and increased between 2013 and 2015.
SHIGA TOXIN-PRODUCING ESCHERICHIA COLI (STEC). Incidence* of reported cases — United States and U.S. territories, 2015
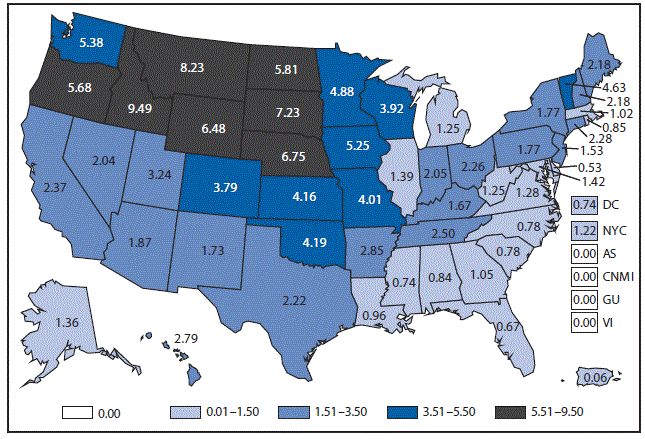
* Per 100,000 population.
Shiga toxin-producing Escherichia coli incidence rates were generally highest in the northern and western states. States with the highest incidence rates were Idaho, Montana, and South Dakota.
SPOTTED FEVER RICKETTSIOSIS. Number of reported cases, by county — United States, 2015
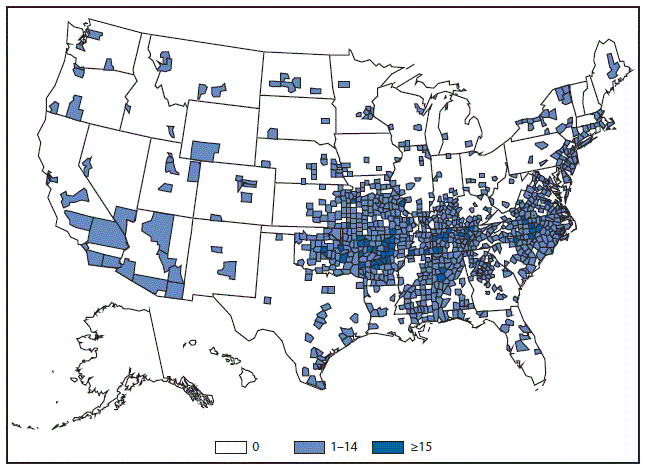
Most spotted fever rickettsiosis cases originating in the United States are attributed to infection with Rickettsia rickettsii (the causative agent for Rocky Mountain spotted fever). However, rickettsioses caused by other spotted fevers including Rickettsia parkeri, Rickettsia species 364D (provisionally called Rickettsia philipii) and Rickettsia akari are being diagnosed and reported more frequently.
TRICHINELLOSIS. Number of reported cases, by year — United States, 1985–2015
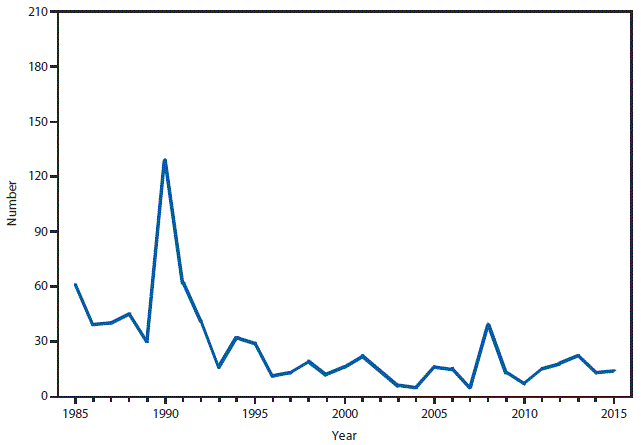
In 2015, a total of 13 trichinellosis cases were reported. This number differs from the denominator of 14 cases presented in the tables; one case from Wisconsin was reclassified as suspect from confirmed, which was not changed before the deadline for finalizing data. Two outbreaks of three cases each occurred in persons who consumed black bear hunted in Alaska. Overall, a majority of reported trichinellosis cases occurred in persons with a history of consumption of undercooked wild game meat.
TUBERCULOSIS. Incidence* of reported cases — United States and U.S. territories, 2015
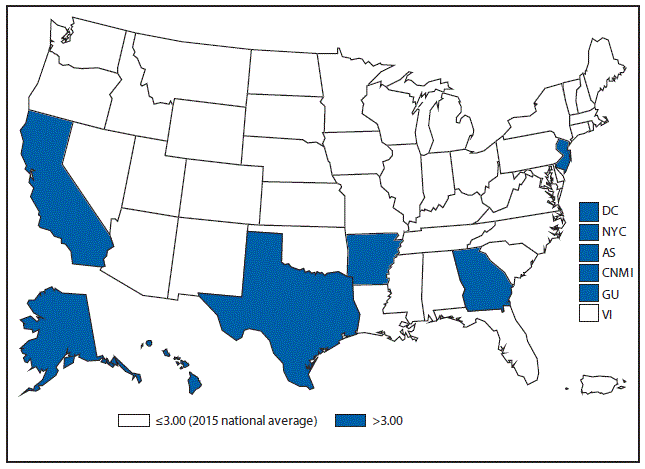
* Per 100,000 population.
Seven states, New York City, the District of Columbia, and three territories (American Samoa, the Commonwealth of the Northern Mariana Islands, and Guam) had a tuberculosis incidence rate above the national average of 3.0 cases per 100,000 population.
TUBERCULOSIS. Incidence* of reported cases, by race/ethnicity — United States, 2005–2015
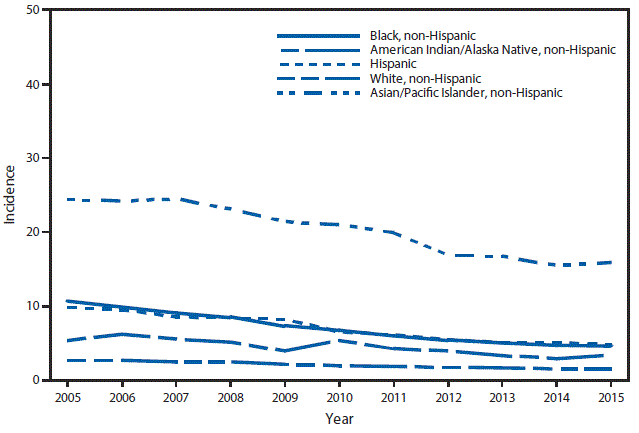
* Per 100,000 population. Data from the Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention.
After approximately 20 consecutive years of declining tuberculosis incidence, the decline in incidence for most race/ethnicities has slowed over the past few years.
TUBERCULOSIS. Number* of reported cases among U.S.-born and foreign-born persons,† by year — United States, 2005–2015
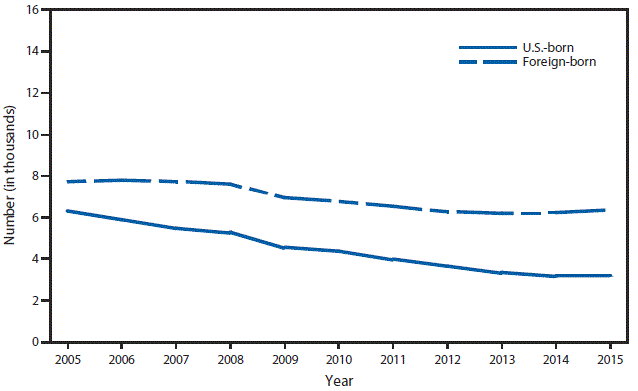
* Number represented is in thousands. Data from the Division of Tuberculosis Elimination, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention.
† For 2015, the origin of birth for 18 patients was unknown.
The number of U.S.-born tuberculosis cases was similar in 2015, compared with 2014, after consistent declines since 2005, while the number of foreign-born cases increased slightly.
TULAREMIA. Number of reported cases — United States and U.S. territories, 2015
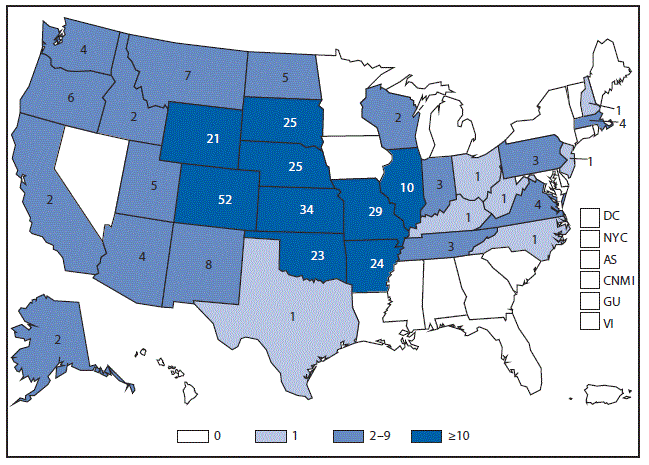
In 2015, a total of 314 cases of tularemia were reported to CDC, the most since 1964. The majority of cases were reported from states in the central United States; cases reported from Colorado, Nebraska, South Dakota and Wyoming increased substantially compared with 2014.
TYPHOID FEVER. Incidence* of reported cases, by year — United States, 1985–2015
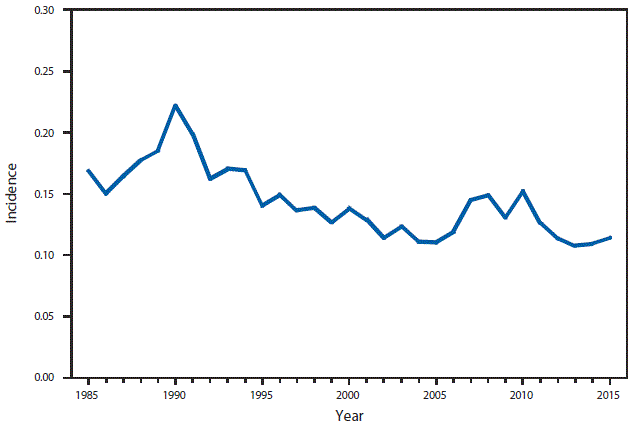
* Per 100,000 population.
In the United States, typhoid fever remains primarily a disease of travelers to countries where typhoid fever is endemic, for whom vaccination against typhoid fever is recommended. During the last 30 years, the annual number of typhoid fever cases peaked in 1990 (552 cases; 0.22 per 100,000) and then declined to a low of 321 (0.11 per 100,000) cases in 2002. Case counts then returned to levels observed in the early 1990s, followed by a 5% increase from 349 (0.11 per 100,000) in 2014 to 367 in 2015 (0.11 per 100,000).
VARICELLA (CHICKENPOX). Number of reported cases — Illinois, Michigan, Texas, and West Virginia, 1993–2015
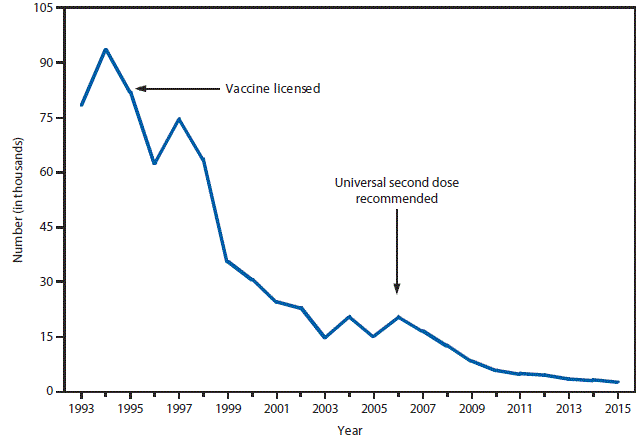
In four states (Illinois, Michigan, Texas, and West Virginia), the number of varicella cases reported in 2015 was 15.5% lower than 2014, 87.6% lower than the average annual number reported during the mature 1-dose varicella vaccination era of 2000–2006, and 96.9% lower than the average annual number reported during the prevaccine years of 1993–1995.
VIBRIOSIS. Number of reported cases — United States and U.S. territories, 2015
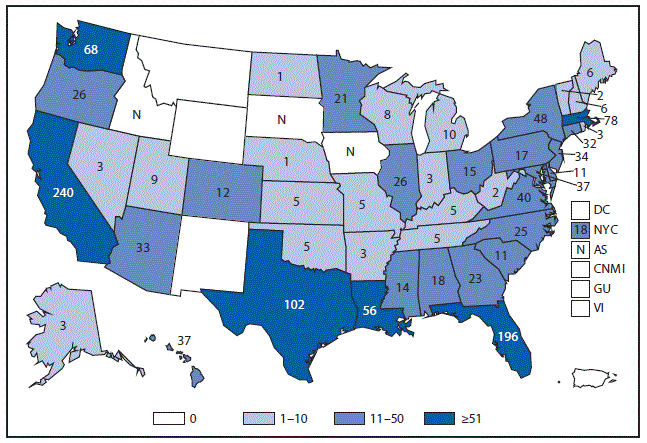
Abbreviation: N = not reportable.
In 2015, a total of 1,323 cases of vibriosis were reported. California, Florida, Texas, and Massachusetts reported the greatest number of cases.
Selected Reading for 2015
General
Adekoya N, Truman BI, Ajani UA. Completeness of reporting of race and ethnicity data in the nationally notifiable diseases surveillance system, United States, 2006–2010. J Public Health Manag Pract 2015;21:E16–22. CrossRefexternal icon PubMedexternal icon
Adams DA, Thomas KR, Jajosky RA, et al. Summary of notifiable infectious diseases and conditions—United States, 2014. MMWR Morb Mortal Wkly Rep 2016;63. CrossRefexternal icon
Beltran VM, Harrison KM, Hall HI, Dean HD. Collection of social determinant of health measures in U.S. national surveillance systems for HIV, viral hepatitis, STDs, and TB. Public Health Rep 2011;126(Suppl 3):41–53. PubMedexternal icon
Blau DM, Clark SC, Nolte KB; National Association of Medical Examiners Ad-hoc Committee for Bioterrorism and Infectious Diseases. Infectious disease surveillance by medical examiners and coroners. Emerg Infect Dis 2013;19:821–2. CrossRefexternal icon PubMedexternal icon
Boehmer TK, Patnaik JL, Burnite SJ, Ghosh TS, Gershman K, Vogt RL. Use of hospital discharge data to evaluate notifiable disease reporting to Colorado’s Electronic Disease Reporting System. Public Health Rep 2011;126:100–6. PubMedexternal icon
Buehler JW, Hopkins RS, Overhage JM, Sosin DM, Tong V; CDC Working Group. Framework for evaluating public health surveillance systems for early detection of outbreaks: recommendations from the CDC Working Group. MMWR Recomm Rep 2004;53(No. RR-5):1–11. PubMedexternal icon
CDC. CDC’s vision for public health surveillance in the 21st century. MMWR Suppl 2012;2012:61(July 27, 2012).
CDC. Comparison of provisional with final notifiable disease case counts—National Notifiable Diseases Surveillance System, 2009. MMWR Morb Mortal Wkly Rep 2013;62:747–51. PubMedexternal icon
Adekoya N, Truman B, Landen M. Incidence of notifiable diseases among American Indians/Alaska Natives—United States, 2007–2011. MMWR Morb Mortal Wkly Rep 2015;64:16–9. PubMedexternal icon
CDC. Manual for the surveillance of vaccine-preventable diseases. 6th ed. Atlanta, GA: US Department of Health and Human Services, CDC; 2013. https://www.cdc.gov/vaccines/pubs/surv-manual/index.html
National Electronic Disease Surveillance System Working Group. National Electronic Disease Surveillance System (NEDSS): a standards-based approach to connect public health and clinical medicine. J Public Health Manag Pract 2001;7:43–50. CrossRefexternal icon PubMedexternal icon
CDC. National Notifiable Diseases Surveillance System (NNDSS). Atlanta, GA: US Department of Health and Human Services, CDC; 2015. https://wwwn.cdc.gov/nndss
CDC. NNDSS Modernization Initiative (NMI). Atlanta, GA: US Department of Health and Human Services, CDC; 2017. https://www.cdc.gov/nmi/index.html
CDC. Potential effects of electronic laboratory reporting on improving timeliness of infectious disease notification—Florida, 2002–2006. MMWR Morb Mortal Wkly Rep 2008;57:1325–8. PubMedexternal icon
CDC. Reporting race and ethnicity data—National Electronic Telecommunications System for Surveillance, 1994–1997. MMWR Morb Mortal Wkly Rep 1999;48:305–12. PubMedexternal icon
CDC. State electronic disease surveillance systems—United States, 2007 and 2010. MMWR Morb Mortal Wkly Rep 2011;60:1421–3. PubMedexternal icon
German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, Waller MN; Guidelines Working Group. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep 2001;50(No. RR-13):1–35, quiz CE1–7. PubMedexternal icon
Lamb E, Satre J, Hurd-Kundeti G, et al. Update on progress in electronic reporting of laboratory results to public health agencies—United States, 2014. MMWR Morb Mortal Wkly Rep 2015;64:328–30. PubMedexternal icon
CDC. Use of race and ethnicity in public health surveillance: summary of the CDC/ATSDR workshop. MMWR Recomm Rep 1993;42(No. RR-10).
Cronquist AB, Mody RK, Atkinson R, et al. Impacts of culture-independent diagnostic practices on public health surveillance for bacterial enteric pathogens. Clin Infect Dis 2012;54(Suppl 5):S432–9. CrossRefexternal icon PubMedexternal icon
Dato V, Wagner MM, Fapohunda A. How outbreaks of infectious disease are detected: a review of surveillance systems and outbreaks. Public Health Rep 2004;119:464–71. CrossRefexternal icon PubMedexternal icon
Dixon BE, Siegel JA, Oemig TV, Grannis SJ. Electronic health information quality challenges and interventions to improve public health surveillance data and practice. Public Health Rep 2013;128:546–53. PubMedexternal icon
Effler P, Ching-Lee M, Bogard A, Ieong MC, Nekomoto T, Jernigan D. Statewide system of electronic notifiable disease reporting from clinical laboratories: comparing automated reporting with conventional methods. JAMA 1999;282:1845–50. CrossRefexternal icon PubMedexternal icon
Fairchild A, Bayer R, Colgrove J. Privacy and public health surveillance: the enduring tension. Virtual Mentor 2007;9:838–41. CrossRefexternal icon PubMedexternal icon
Friedman DJ, Parrish RG, Ross DA. Electronic health records and US public health: current realities and future promise. Am J Public Health 2013;103:1560–7. CrossRefexternal icon PubMedexternal icon
German RR. Sensitivity and predictive value positive measurements for public health surveillance systems. Epidemiology 2000;11:720–7. CrossRefexternal icon PubMedexternal icon
Greene SK, Peterson ER, Kapell D, Fine AD, Kulldorff M. Daily reportable disease spatiotemporal cluster detection, New York City, New York, USA, 2014–2015. Emerg Infect Dis 2016;22:1808–12. CrossRefexternal icon PubMedexternal icon
Government Accountability Office. Emerging infectious diseases: review of state and federal disease surveillance efforts. Washington, DC: Government Accountability Office; 2004. GAO-04-877. http://www.gao.gov/new.items/d04877.pdfpdf iconexternal icon
Heymann DL, editor. Control of communicable diseases manual. 20th ed. Washington, DC: American Public Health Association; 2014.
Hopkins RS. Design and operation of state and local infectious disease surveillance systems. J Public Health Manag Pract 2005;11:184–90. CrossRefexternal icon PubMedexternal icon
Jajosky RA, Groseclose SL. Evaluation of reporting timeliness of public health surveillance systems for infectious diseases. BMC Public Health 2004;4:29. CrossRefexternal icon PubMedexternal icon
Krause G, Brodhun B, Altmann D, Claus H, Benzler J. Reliability of case definitions for public health surveillance assessed by Round-Robin test methodology. BMC Public Health 2006;6:129. CrossRefexternal icon PubMedexternal icon
Lazarus R, Klompas M, Campion FX, et al. Electronic Support for Public Health: validated case finding and reporting for notifiable diseases using electronic medical data. J Am Med Inform Assoc 2009;16:18–24. CrossRefexternal icon PubMedexternal icon
Lee LM, Teutsch SM, Thacker SB, St Louis ME, eds. Principles and practice of public health surveillance. 3rd ed. New York, NY: Oxford University Press; 2010:1–17.
Lee LM, Thacker SB. The cornerstone of public health practice: public health surveillance, 1961–2011. MMWR Surv Summ 2011;60(No. Suppl 4):15–21.
Levin-Rector A, Wilson EL, Fine AD, Greene SK. Refining historical limits method to improve disease cluster detection, New York City, New York, USA. Emerg Infect Dis 2015;21:265–72. CrossRefexternal icon PubMedexternal icon
Jajosky RA, Ward J. National, state, and local public health surveillance systems. In: M’ikanatha NM, Iskander J, eds. Concepts and methods in infectious disease surveillance. Hoboken, NJ: Wiley; 2015.
M’ikanatha NM, Lynfield R, Van Beneden CA, de Valk H. Infectious disease surveillance. 2nd ed. Malden, MA: Wiley; 2013.
Nguyen TQ, Thorpe L, Makki HA, Mostashari F. Benefits and barriers to electronic laboratory results reporting for notifiable diseases: the New York City Department of Health and Mental Hygiene experience. Am J Public Health 2007;97(Suppl 1):S142–5. CrossRefexternal icon PubMedexternal icon
Overhage JM, Grannis S, McDonald CJ. A comparison of the completeness and timeliness of automated electronic laboratory reporting and spontaneous reporting of notifiable conditions. Am J Public Health 2008;98:344–50. CrossRefexternal icon PubMedexternal icon
Pickering LK, ed. Red Book: 2015 Report of the Committee on Infectious Diseases. 30th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2015.
Roush SW, Murphy TV; Vaccine-Preventable Disease Table Working Group. Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA 2007;298:2155–63. CrossRefexternal icon PubMedexternal icon
Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
Sickbert-Bennett EE, Weber DJ, Poole C, MacDonald PD, Maillard JM. Completeness of communicable disease reporting, North Carolina, USA, 1995–1997 and 2000–2006. Emerg Infect Dis 2011;17:23–9. CrossRefexternal icon PubMedexternal icon
Silk BJ, Berkelman RL. A review of strategies for enhancing the completeness of notifiable disease reporting. J Public Health Manag Pract 2005;11:191–200. CrossRefexternal icon PubMedexternal icon
Struelens MJ, Brisse S. From molecular to genomic epidemiology: transforming surveillance and control of infectious diseases. Euro Surveill 2013;18:20386. PubMedexternal icon
Vogel J, Brown JS, Land T, Platt R, Klompas M. MDPHnet: secure, distributed sharing of electronic health record data for public health surveillance, evaluation, and planning. Am J Public Health 2014;104:2265–70. CrossRefexternal icon PubMedexternal icon
Zhou H, Burkom H, Katz S, et al. Comparing historical limits method with regression model for weekly monitoring of notifiable diseases, Seattle, WA, August 8–13, 2015, Joint Statistical Meetings, and Published on the JSM Conference proceeding, 2015.
Anthrax
Bower W, Hendricks K, Pillai S, Guarnizo J, Meaney-Delman D. Clinical framework and medical countermeasure use during an anthrax mass-casualty incident: CDC recommendations. MMWR Recomm Rep 2015;64(No. RR-4).
Bradley JS, Peacock G, Krug SE, et al. ; AAP Committee on Infectious Diseases and Disaster Preparedness Advisory Council. Pediatric anthrax clinical management. Pediatrics 2014;133:e1411–36. CrossRefexternal icon PubMedexternal icon
Hendricks KA, Wright ME, Shadomy SV, et al. ; Workgroup on Anthrax Clinical Guidelines. Centers for disease control and prevention expert panel meetings on prevention and treatment of anthrax in adults. Emerg Infect Dis 2014;20: . CrossRefexternal icon PubMedexternal icon
Katharios-Lanwermeyer S, Holty JE, Person M, et al. Identifying meningitis during an anthrax mass casualty incident: systematic review of systemic anthrax since 1880. Clin Infect Dis 2016;62:1537–45. CrossRefexternal icon PubMedexternal icon
Meaney-Delman D, Zotti ME, Creanga AA, et al. ; Workgroup on Anthrax in Pregnant and Postpartum Women. Special considerations for prophylaxis for and treatment of anthrax in pregnant and postpartum women. Emerg Infect Dis 2014;20:e130611. CrossRefexternal icon PubMedexternal icon
Pillai SK, Huang E, Guarnizo JT, et al. Antimicrobial treatment for systemic anthrax: analysis of cases from 1945 to 2014 identified through a systematic literature review. Health Secur 2015;13:355–64. CrossRefexternal icon PubMedexternal icon
Arboviral, Neuroinvasive and Nonneuroinvasive
Gaensbauer JT, Lindsey NP, Messacar K, Staples JE, Fischer M. Neuroinvasive arboviral disease in the United States: 2003 to 2012. Pediatrics 2014;134:e642–50. CrossRefexternal icon PubMedexternal icon
Hahn MB, Monaghan AJ, Hayden MH, et al. Meteorological conditions associated with increased incidence of West Nile virus disease in the United States, 2004–2012. Am J Trop Med Hyg 2015;92:1013–22. CrossRefexternal icon PubMedexternal icon
Healy JM, Reisen WK, Kramer VL, et al. Comparison of the efficiency and cost of West Nile virus surveillance methods in California. Vector Borne Zoonotic Dis 2015;15:147–55. CrossRefexternal icon PubMedexternal icon
Krow-Lucal E, Lindsey NP, Lehman J, Fischer M, Staples JE. West Nile virus and other nationally notifiable arboviral diseases—United States, 2015. MMWR Morb Mortal Wkly Rep 2017;66:51–5. CrossRefexternal icon PubMedexternal icon
Lindsey NP, Fischer M, Neitzel D, et al. Hospital-based enhanced surveillance for West Nile virus neuroinvasive disease. Epidemiol Infect 2016;1:1–6. PubMedexternal icon
Lindsey NP, Prince HE, Kosoy O, et al. Chikungunya virus infections among travelers-United States, 2010–2013. Am J Trop Med Hyg 2015;92:82–7. CrossRefexternal icon PubMedexternal icon
Lindsey NP, Staples JE, Delorey MJ, Fischer M. Lack of evidence of increased West Nile virus disease severity in the United States in 2012. Am J Trop Med Hyg 2014;90:163–8. CrossRefexternal icon PubMedexternal icon
Lindsey NP, Staples JE, Lehman JA, Fischer M. Surveillance for West Nile virus disease—United States, 1999–2008. MMWR Surv Summ 2010;59(No. SS-2).
Pastula DM, Hoang Johnson DK, White JL, Dupuis AP 2nd, Fischer M, Staples JE. Jamestown Canyon virus disease in the United States—2000–2013. Am J Trop Med Hyg 2015;93:384–9. CrossRefexternal icon PubMedexternal icon
Reimann CA, Hayes EB, DiGuiseppi C, et al. Epidemiology of neuroinvasive arboviral disease in the United States, 1999–2007. Am J Trop Med Hyg 2008;79:974–9. PubMedexternal icon
Staples JE, Shankar MB, Sejvar JJ, Meltzer MI, Fischer M. Initial and long-term costs of patients hospitalized with West Nile virus disease. Am J Trop Med Hyg 2014;90:402–9. CrossRefexternal icon PubMedexternal icon
Venkat H, Krow-Lucal E, Hennessey M, et al. Notes from the field: concurrent outbreaks of St. Louis encephalitis virus and West Nile virus disease—Arizona, 2015. MMWR Morb Mortal Wkly Rep 2015;64:1349–50. PubMedexternal icon
Yendell SJ, Fischer M, Staples JE. Colorado tick fever in the United States, 2002–2012. Vector Borne Zoonotic Dis 2015;15:311–6. CrossRefexternal icon PubMedexternal icon
Babesiosis
Acosta ME, Ender PT, Smith EM, Jahre JA. Babesia microti infection, eastern Pennsylvania, USA. Emerg Infect Dis 2013;19:1105–7. CrossRefexternal icon PubMedexternal icon
CDC. Babesiosis surveillance—18 states, 2011. MMWR Morb Mortal Wkly Rep 2012;61:505–9. PubMedexternal icon
Herwaldt BL, Linden JV, Bosserman E, Young C, Olkowska D, Wilson M. Transfusion-associated babesiosis in the United States: a description of cases. Ann Intern Med 2011;155:509–19. CrossRefexternal icon PubMedexternal icon
Joseph JT, Purtill K, Wong SJ, et al. Vertical transmission of Babesia microti, United States. Emerg Infect Dis 2012;18:1318–21. CrossRefexternal icon PubMedexternal icon
Vannier E, Krause PJ. Human babesiosis. N Engl J Med 2012;366:2397–407. CrossRefexternal icon PubMedexternal icon
Botulism
Arnon SS, Barzilay EJ. Clostridial infections: botulism and infant botulism. In: Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. Red Book: 2009 report of the Committee on Infectious Diseases. Elk Grove Village, IL: American Academy of Pediatrics; 2009:259–62.
CDC. Infant botulism—New York City, 2001–2002. MMWR Morb Mortal Wkly Rep 2003;52:21–4. PubMedexternal icon
Fagan RP, McLaughlin JB, Castrodale LJ, et al. Endemic foodborne botulism among Alaska Native persons—Alaska, 1947–2007. Clin Infect Dis 2011;52:585–92. CrossRefexternal icon PubMedexternal icon
Newkirk RW, Hedberg CW. Rapid detection of foodborne botulism outbreaks facilitated by epidemiological linking of cases: implications for food defense and public health response. Foodborne Pathog Dis 2012;9:150–5. CrossRefexternal icon PubMedexternal icon
Rao A, Jackson KA. Botulism. In: DL Heymann, ed. Control of communicable diseases manual. Washington, DC: American Public Health Association Press; 2015.
Sobel S. Botulism. Clin Infect Dis 2005;41:1167–73. CrossRefexternal icon PubMedexternal icon
Sobel J, Tucker N, Sulka A, McLaughlin J, Maslanka S. Foodborne botulism in the United States, 1990–2000. Emerg Infect Dis 2004;10:1606–11. CrossRefexternal icon PubMedexternal icon
Shapiro RL, Hatheway C, Becher J, Swerdlow DL. Botulism surveillance and emergency response. A public health strategy for a global challenge. JAMA 1997;278:433–5. CrossRefexternal icon PubMedexternal icon
Shapiro RL, Hatheway C, Swerdlow DL. Botulism in the United States: a clinical and epidemiologic review. Ann Intern Med 1998;129:221–8. CrossRefexternal icon PubMedexternal icon
Werner SB, Passaro D, McGee J, Schechter R, Vugia DJ. Wound botulism in California, 1951–1998: recent epidemic in heroin injectors. Clin Infect Dis 2000;31:1018–24. CrossRefexternal icon PubMedexternal icon
Brucellosis
Ashford DA, di Pietra J, Lingappa J, et al. Adverse events in humans associated with accidental exposure to the livestock brucellosis vaccine RB51. Vaccine 2004;22:3435–9. CrossRefexternal icon PubMedexternal icon
CDC. Brucellosis. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. https://www.cdc.gov/nczved/divisions/dfbmd/diseases/brucellosis
CDC. Brucellosis (Brucella melitensis, abortus, suis, and canis). Atlanta, GA: US Department of Health and Human Services, CDC; 2012.
CDC. Brucellosis case definition. Atlanta, GA: US Department of Health and Human Services, CDC; 2010. https://wwwn.cdc.gov/nndss/conditions/brucellosis/case-definition/2010
CDC. Brucella suis infection associated with feral swine hunting—three states, 2007-2008. MMWR Morb Mortal Wkly Rep 2009;58:618–21. PubMedexternal icon
CDC. Laboratory-acquired brucellosis—Indiana and Minnesota, 2006. MMWR Morb Mortal Wkly Rep 2008;57:39–42. PubMedexternal icon
CDC. Public health consequences of a false-positive laboratory test result for Brucella—Florida, Georgia, and Michigan, 2005. MMWR Morb Mortal Wkly Rep 2008;57:603–5. PubMedexternal icon
Glynn MK, Lynn TV. Brucellosis. J Am Vet Med Assoc 2008;233:900–8. CrossRefexternal icon PubMedexternal icon
Traxler RM, Lehman MW, Bosserman EA, Guerra MA, Smith TL. A literature review of laboratory-acquired brucellosis. J Clin Microbiol 2013;51:3055–62. CrossRefexternal icon PubMedexternal icon
Yagupsky P, Baron EJ. Laboratory exposures to brucellae and implications for bioterrorism. Emerg Infect Dis 2005;11:1180–5. CrossRefexternal icon PubMedexternal icon
Campylobacteriosis
Davis KR, Dunn AC, Burnett C, et al. Campylobacter jejuni infections associated with raw milk consumption—Utah, 2014. MMWR Morb Mortal Wkly Rep 2016;65:301–5. CrossRefexternal icon PubMedexternal icon
CDC. Multistate outbreak of Campylobacter jejuni infections associated with undercooked chicken livers—northeastern United States, 2012. MMWR Morb Mortal Wkly Rep 2013;62:874–6. PubMedexternal icon
Noormohamed A, Fakhr MK. Incidence and antimicrobial resistance profiling of Campylobacter in retail chicken livers and gizzards. Foodborne Pathog Dis 2012;9:617–24. CrossRefexternal icon PubMedexternal icon
Ailes E, Scallan E, Berkelman RL, Kleinbaum DG, Tauxe RV, Moe CL. Do differences in risk factors, medical care seeking, or medical practices explain the geographic variation in campylobacteriosis in Foodborne Diseases Active Surveillance Network (FoodNet) sites? Clin Infect Dis 2012;54(Suppl 5):S464–71. CrossRefexternal icon PubMedexternal icon
Samuel MC, Vugia DJ, Shallow S, et al. ; Emerging Infections Program FoodNet Working Group. Epidemiology of sporadic Campylobacter infection in the United States and declining trend in incidence, FoodNet 1996–1999. Clin Infect Dis 2004;38(Suppl 3):S165–74. CrossRefexternal icon PubMedexternal icon
Chlamydia trachomatis Infection
CDC. Sexually transmitted disease surveillance, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016.
Lee KC, Ngo-Metzger Q, Wolff T, Chowdhury J, LeFevre ML, Meyers DS. Sexually transmitted infections: recommendations from the U.S. Preventive Services Task Force. Am Fam Physician 2016;94:907–15. PubMedexternal icon
Satterwhite CL, Torrone E, Meites E, et al. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis 2013;40:187–93. CrossRefexternal icon PubMedexternal icon
Torrone E, Papp J, Weinstock H. Prevalence of Chlamydia trachomatis genital infection among persons aged 14–39 years—United States, 2007–2012. MMWR Morb Mortal Wkly Rep 2014;63:834–8. PubMedexternal icon
Cholera
Besser RE, Feikin DR, Eberhart-Phillips JE, Mascola L, Griffin PM. Diagnosis and treatment of cholera in the United States. Are we prepared? JAMA 1994;272:1203–5. CrossRefexternal icon PubMedexternal icon
Loharikar A, Newton AE, Stroika S, et al. Cholera in the United States, 2001–2011: a reflection of patterns of global epidemiology and travel. Epidemiol Infect 2015;143:695–9. CrossRefexternal icon PubMedexternal icon
Mintz ED, Guerrant RL. A lion in our village—the unconscionable tragedy of cholera in Africa. N Engl J Med 2009;360:1060–3. CrossRefexternal icon PubMedexternal icon
Newton AE, Heiman KE, Schmitz A, et al. Cholera in United States associated with epidemic in Hispaniola. Emerg Infect Dis 2011;17:2166–8. CrossRefexternal icon PubMedexternal icon
Siddique AK, Nair GB, Alam M, et al. El Tor cholera with severe disease: a new threat to Asia and beyond. Epidemiol Infect 2010;138:347–52. CrossRefexternal icon PubMedexternal icon
Steinberg EB, Greene KD, Bopp CA, Cameron DN, Wells JG, Mintz ED. Cholera in the United States, 1995–2000: trends at the end of the twentieth century. J Infect Dis 2001;184:799–802. CrossRefexternal icon PubMedexternal icon
Tappero JW, Tauxe RV. Lessons learned during public health response to cholera epidemic in Haiti and the Dominican Republic. Emerg Infect Dis 2011;17:2087–93. CrossRefexternal icon PubMedexternal icon
World Health Organization. Cholera, 2012. Wkly Epidemiol Rec 2013;88:321–34. PubMedexternal icon
Coccidioidomycosis
Engelthaler DM, Roe CC, Hepp CM, et al. local population structure and patterns of western hemisphere dispersal for Coccidioides spp., the fungal cause of valley fever. MBio 2016;7:e00550-16. CrossRefexternal icon PubMedexternal icon
Galgiani JN, Ampel NM, Blair JE, et al. 2016 Infectious Diseases Society of America (IDSA) clinical practice guideline for the treatment of Coccidioidomycosis. Clin Infect Dis 2016;63:e112–46. CrossRefexternal icon PubMedexternal icon
Sondermeyer GL, Lee LA, Gilliss D, Vugia DJ. Coccidioidomycosis-associated deaths in California, 2000–2013. Public Health Rep 2016;131:531–5. CrossRefexternal icon PubMedexternal icon
Cryptosporidiosis
CDC. CryptoNet: molecular-based tracking to better understand U.S. Cryptosporidium transmission. Atlanta, GA: US Department of Health and Human Services, CDC; 2013. https://www.cdc.gov/parasites/crypto/cryptonet.html
CDC. DPDx: Laboratory identification of parasitic diseases of public health concern: diagnostic procedures for cryptosporidiosis. Atlanta, GA: US Department of Health and Human Services, CDC; 2013. https://www.cdc.gov/dpdx/diagnosticProcedures/stool/antigendetection.html
Hlavsa MC, Roberts VA, Kahler AM, et al. Outbreaks of illness associated with recreational water—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2015;64:668–72. PubMedexternal icon
Painter JE, Gargano JW, Yoder JS, Collier SA, Hlavsa MC. Evolving epidemiology of reported cryptosporidiosis cases in the United States, 1995–2012. Epidemiol Infect 2016;144:1792–802. CrossRefexternal icon PubMedexternal icon
Painter JE, Hlavsa MC, Collier SA, Xiao L, Yoder JS. Cryptosporidiosis surveillance—United States, 2011-2012. MMWR Suppl 2015;64(No. SS-3):1–14. PubMedexternal icon
Roy SL, DeLong SM, Stenzel SA, et al. ; Emerging Infections Program FoodNet Working Group. Risk factors for sporadic cryptosporidiosis among immunocompetent persons in the United States from 1999 to 2001. J Clin Microbiol 2004;42:2944–51. CrossRefexternal icon PubMedexternal icon
Cyclosporiasis
Abanyie F, Harvey RR, Harris JR, et al. ; Multistate Cyclosporiasis Outbreak Investigation Team. 2013 multistate outbreaks of Cyclospora cayetanensis infections associated with fresh produce: focus on the Texas investigations. Epidemiol Infect 2015;143:3451–8. CrossRefexternal icon PubMedexternal icon
Hall RL, Jones JL, Herwaldt BL. Surveillance for laboratory-confirmed sporadic cases of cyclosporiasis—United States, 1997–2008. MMWR Surveill Summ 2011;60(No. SS-2):1–11. PubMedexternal icon
Hall RL, Jones JL, Hurd S, Smith G, Mahon BE, Herwaldt BL. Population-based active surveillance for Cyclospora infection—United States, Foodborne Diseases Active Surveillance Network (FoodNet), 1997–2009. Clin Infect Dis 2012;54(Suppl 5):S411–7. CrossRefexternal icon PubMedexternal icon
Herwaldt BL. Cyclospora cayetanensis: a review, focusing on the outbreaks of cyclosporiasis in the 1990s. Clin Infect Dis 2000;31:1040–57. CrossRefexternal icon PubMedexternal icon
Herwaldt BL. The ongoing saga of U.S. outbreaks of cyclosporiasis associated with imported fresh produce: what Cyclospora cayetanensis has taught us and what we have yet to learn. In: Institute of Medicine. Addressing foodborne threats to health: policies, practices, and global coordination. Washington, DC: The National Academies Press; 2006:85–115, 133–40.
Dengue
Simmons CP, Farrar JJ, Nguyen V, Wills B. Dengue. N Engl J Med 2012;366:1423–32. CrossRefexternal icon PubMedexternal icon
Stanaway JD, Shepard DS, Undurraga EA, et al. The global burden of dengue: an analysis from the Global Burden of Disease Study 2013. Lancet Infect Dis 2016;16:712–23. CrossRefexternal icon PubMedexternal icon
Diphtheria
DeWinter LM, Bernard KA, Romney MG. Human clinical isolates of Corynebacterium diphtheriae and Corynebacterium ulcerans collected in Canada from 1999 to 2003 but not fitting reporting criteria for cases of diphtheria. J Clin Microbiol 2005;43:3447–9. CrossRefexternal icon PubMedexternal icon
Tiwari TW, Wharton M. Diphtheria toxoid In: Plotkin O, Orenstein W, Offitt P, eds. Vaccines. Edinburgh, UK: Saunders, 2012.
Wagner KS, Stickings P, White JM, et al. A review of the international issues surrounding the availability and demand for diphtheria antitoxin for therapeutic use. Vaccine 2009;28:14–20. CrossRefexternal icon PubMedexternal icon
Wagner KS, White JM, Crowcroft NS, De Martin S, Mann G, Efstratiou A. Diphtheria in the United Kingdom, 1986–2008: the increasing role of Corynebacterium ulcerans. Epidemiol Infect 2010;138:1519–30. CrossRefexternal icon PubMedexternal icon
Wagner KS, White JM, Lucenko I, et al. ; Diphtheria Surveillance Network. Diphtheria in the postepidemic period, Europe, 2000–2009. Emerg Infect Dis 2012;18:217–25. CrossRefexternal icon PubMedexternal icon
Zakikhany K, Efstratiou A. Diphtheria in Europe: current problems and new challenges. Future Microbiol 2012;7:595–607. CrossRefexternal icon PubMedexternal icon
Ehrlichiosis and Anaplasmosis
CDC. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States: a practical guide for health care and public health professionals. MMWR Recomm Rep 2016;65(No. RR-2).
Dahlgren FS, Heitman KN, Drexler NA, Massung RF, Behravesh CB. Human granulocytic anaplasmosis in the United States from 2008 to 2012: a summary of national surveillance data. Am J Trop Med Hyg 2015;93:66–72. CrossRefexternal icon PubMedexternal icon
Dahlgren FS, Nichols Heitman K, Drexler N, Massung RF, Barton Behravesh C. Undetermined ehrlichiosis and anaplasmosis in the United States, 2008–2012: a catch-all for passive surveillance. Am J Trop Med Hyg 2016;94:299–301. CrossRefexternal icon PubMedexternal icon
Harris RM, Couturier BA, Sample SC, Coulter KS, Casey KK, Schlaberg R. Expanded geographic distribution and clinical characteristics of Ehrlichia ewingii infections, United States. Emerg Infect Dis 2016;22:862–5. CrossRefexternal icon PubMedexternal icon
Johnson DK, Schiffman EK, Davis JP, et al. Human infection with Ehrlichia muris-like pathogen, United States, 2007–2013. Emerg Infect Dis 2015;21:1794–9. CrossRefexternal icon PubMedexternal icon
Nichols Heitman K, Dahlgren FS, Drexler NA, Massung RF, Behravesh CB. Increasing incidence of Ehrlichiosis in the United States: a summary of national surveillance of Ehrlichia chaffeensis and Ehrlichia ewingii infections in the United States, 2008–2012. Am J Trop Med Hyg 2016;94:52–60. CrossRefexternal icon PubMedexternal icon
Giardiasis
Adam EA, Yoder JS, Gould H, Hlavsa MC. Giardiasis outbreaks in the United States, 1971–2011. Epidemiol Infect 2016. https://www.ncbi.nlm.nih.gov/pubmed/26750152external icon
Anonymous. Drugs for parasitic infections. Treat Guidel Med Lett 2010;8:e5.
Cantey PT, Roy S, Lee B, et al. Study of nonoutbreak giardiasis: novel findings and implications for research. Am J Med 2011;124:1175.e1–8. CrossRefexternal icon PubMedexternal icon
Clinical and Laboratory Standards Institute. Procedures for the recovery and identification of parasites from the intestinal tract; approved guideline. CLSI document M28-A2, 2nd ed. Wayne, PA: Clinical and Laboratory Standards Institute; 2005.
Gonorrhea
CDC. Sexually transmitted disease surveillance, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016. https://www.cdc.gov/std/stats15/default.htm
LeFevre ML; U.S. Preventive Services Task Force. Screening for Chlamydia and gonorrhea: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2014;161:902–10. CrossRefexternal icon PubMedexternal icon
Torrone EA, Johnson RE, Tian LH, Papp JR, Datta SD, Weinstock HS. Prevalence of Neisseria gonorrhoeae among persons 14 to 39 years of age, United States, 1999 to 2008. Sex Transm Dis 2013;40:202–5. CrossRefexternal icon PubMedexternal icon
Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3):1–137. PubMedexternal icon
Haemophilus influenzae
Blain, A, MacNeil, J, Wang, X et al. Invasive Haemophilus influenzae disease in adults ≥65 years, United States, 2011. Open Forum Infectious Diseases 2014;1:ofuo44.
Briere EC, Jackson M, Shah SG, et al. Haemophilus influenzae type b disease and vaccine booster dose deferral, United States, 1998–2009. Pediatrics 2012;130:414–20. CrossRefexternal icon PubMedexternal icon
Briere EC, Rubin L, Moro PL, Cohn A, Clark T, Messonnier N. Prevention and control of haemophilus influenzae type b disease: recommendations of the advisory committee on immunization practices (ACIP). MMWR Recomm Rep 2014;63(No. RR-1):1–14. PubMedexternal icon
MacNeil JR, Cohn AC, Farley M, et al. Current epidemiology and trends in invasive Haemophilus influenzae disease—United States, 1989-2008. Clin Infect Dis 2011;53:1230–6. CrossRefexternal icon PubMedexternal icon
Schuchat A, Messonnier NR. From pandemic suspect to the postvaccine era: the Haemophilus influenzae story. Clin Infect Dis 2007;44:817–9. CrossRefexternal icon PubMedexternal icon
Hansen’s Disease (Leprosy)
Britton WJ, Lockwood DN. Leprosy. Lancet 2004;363:1209–19. CrossRefexternal icon PubMedexternal icon
Hartzell JD, Zapor M, Peng S, Straight T. Leprosy: a case series and review. South Med J 2004;97:1252–6. CrossRefexternal icon PubMedexternal icon
Hastings R, editor. Leprosy. 2nd ed. New York, NY: Churchill Livingstone; 1994.
Scollard DM, Adams LB, Gillis TP, Krahenbuhl JL, Truman RW, Williams DL. The continuing challenges of leprosy. Clin Microbiol Rev 2006;19:338–81. CrossRefexternal icon PubMedexternal icon
Scollard D, Stryjewska B. Epidemiology, microbiology, clinical manifestations, and diagnosis of leprosy. UpToDate 2015. http://www.uptodate.com/contents/epidemiology-microbiology-clinical-manifestations-and-diagnosis-of-leprosyexternal icon
Sharma R, Singh P, Loughry WJ, et al. Zoonotic leprosy in the Southeastern United States. Emerg Infect Dis 2015;21:2127–34. CrossRefexternal icon PubMedexternal icon
Woodall P, Scollard D, Rajan L. Hansen disease among Micronesian and Marshallese persons living in the United States. Emerg Infect Dis 2011;17:1202–8. CrossRefexternal icon PubMedexternal icon
Worobec SM. Current approaches and future directions in the treatment of leprosy. Res Rep Trop Med 2012;3:79–91. CrossRefexternal icon
Hemolytic Uremic Syndrome
Gould LH, Demma L, Jones TF, et al. Hemolytic uremic syndrome and death in persons with Escherichia coli O157:H7 infection, foodborne diseases active surveillance network sites, 2000–2006. Clin Infect Dis 2009;49:1480–5. CrossRefexternal icon PubMedexternal icon
Luna-Gierke RE, Wymore K, Sadlowski J, et al. Multiple-aetiology enteric infections involving non-O157 Shiga toxin-producing Escherichia coli—FoodNet, 2001–2010. Zoonoses Public Health 2014;61:492–8. CrossRefexternal icon PubMedexternal icon
Mody RK, Gu W, Griffin PM, et al. Postdiarrheal hemolytic uremic syndrome in United States children: clinical spectrum and predictors of in-hospital death. J Pediatr 2015;166:1022–9. CrossRefexternal icon PubMedexternal icon
Mody RK, Luna-Gierke RE, Jones TF, et al. Infections in pediatric postdiarrheal hemolytic uremic syndrome: factors associated with identifying shiga toxin-producing Escherichia coli. Arch Pediatr Adolesc Med 2012;166:902–9. CrossRefexternal icon PubMedexternal icon
Ong KL, Apostal M, Comstock N, et al. Strategies for surveillance of pediatric hemolytic uremic syndrome: Foodborne Diseases Active Surveillance Network (FoodNet), 2000–2007. Clin Infect Dis 2012;54(Suppl 5):S424–31. CrossRefexternal icon PubMedexternal icon
Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 2005;365:1073–86. PubMedexternal icon
Human Immunodeficiency Virus Diagnoses
CDC. HIV Surveillance Report, 2015. Atlanta, GA: US Department of Health and Human Services; 2016. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdfpdf icon
CDC. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2014. HIV Surveillance Supplemental Report 2016;21(No.4).
Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep 2008;57(No. RR-10):1–12. PubMedexternal icon
CDC. Revised surveillance case definition for HIV infection—United States, 2014. MMWR Recomm Rep 2014;63(No. RR-3):1–10. PubMedexternal icon
Cohen SM, Gray KM, Ocfemia MC, Johnson AS, Hall HI. The status of the National HIV Surveillance System, United States, 2013. Public Health Rep 2014;129:335–41. PubMedexternal icon
Frieden TR, Foti KE, Mermin J. Applying public health principles to the HIV epidemic—how are we doing? N Engl J Med 2015;373:2281–7. CrossRefexternal icon PubMedexternal icon
Influenza-Associated Pediatric Mortality
Bhat N, Wright JG, Broder KR, et al. ; Influenza Special Investigations Team. Influenza-associated deaths among children in the United States, 2003–2004. N Engl J Med 2005;353:2559–67. CrossRefexternal icon PubMedexternal icon
Blanton L, Peacock G, Cox C, Jhung M, Finelli L, Moore C. Neurologic disorders among pediatric deaths associated with the 2009 pandemic influenza. Pediatrics 2012;130:390–6. CrossRefexternal icon PubMedexternal icon
Council of State and Territorial Epidemiologists. Position statement 04-ID-04: Influenza-associated pediatric mortality 2004. Atlanta, GA: Council of State and Territorial Epidemiologists; 2004. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/04-ID-04-FINAL.pdfpdf iconexternal icon
Council of State and Territorial Epidemiologists. Position statement 07-ID-14: Influenza-associated pediatric mortality 2007. Atlanta, GA: Council of State and Territorial Epidemiologists; 2007. http://c.ymcdn.com/sites/www.cste.org/resource/resmgr/PS/07-ID-14.pdfpdf iconexternal icon
Cox CM, Blanton L, Dhara R, Brammer L, Finelli L. 2009 Pandemic influenza A (H1N1) deaths among children—United States, 2009–2010. Clin Infect Dis 2011;52(Suppl 1):S69–74. CrossRefexternal icon PubMedexternal icon
Finelli L, Fiore A, Dhara R, et al. Influenza-associated pediatric mortality in the United States: increase of Staphylococcus aureus coinfection. Pediatrics 2008;122:805–11. CrossRefexternal icon PubMedexternal icon
Guarner J, Paddock CD, Shieh WJ, et al. Histopathologic and immunohistochemical features of fatal influenza virus infection in children during the 2003–2004 season. Clin Infect Dis 2006;43:132–40. CrossRefexternal icon PubMedexternal icon
Peebles PJ, Dhara R, Brammer L, Fry AM, Finelli L. Influenza-associated mortality among children—United States: 2007–2008. Influenza Other Respi Viruses 2011;5:25–31. CrossRefexternal icon PubMedexternal icon
Quandelacy TM, Viboud C, Charu V, Lipsitch M, Goldstein E. Age- and sex-related risk factors for influenza-associated mortality in the United States between 1997–2007. Am J Epidemiol 2014;179:156–67. CrossRefexternal icon PubMedexternal icon
Wong KK, Jain S, Blanton L, et al. Influenza-associated pediatric deaths in the United States, 2004-2012. Pediatrics 2013;132:796–804. CrossRefexternal icon PubMedexternal icon
Invasive Pneumococcal Disease
CDC. Antibiotic resistance threats in the United States, 2013. Atlanta, GA: US Department of Health and Human Services, CDC; 2014. https://www.cdc.gov/drugresistance/threat-report-2013
CDC. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among children aged 6–18 years with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2013;62:521–4. PubMedexternal icon
CDC. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2012;61:816–9. PubMedexternal icon
Kobayashi M, Bennett NM, Gierke R, et al. Intervals between PCV13 and PPSV23 vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2015;64:944–7. CrossRefexternal icon PubMedexternal icon
Moore MR, Link-Gelles R, Schaffner W, et al. Effect of use of 13-valent pneumococcal conjugate vaccine in children on invasive pneumococcal disease in children and adults in the USA: analysis of multisite, population-based surveillance. Lancet Infect Dis 2015;15:301–9. CrossRefexternal icon PubMedexternal icon
Nuorti JP, Whitney CG. Prevention of pneumococcal disease among infants and children—use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2010;(No. RR-11).
Tomczyk S, Bennett NM, Stoecker C, et al. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 2014;63:822–5. PubMedexternal icon
Tomczyk S, Lynfield R, Schaffner W, et al. Prevention of antibiotic-nonsusceptible invasive pneumococcal disease with the 13-valent pneumococcal conjugate vaccine. Clin Infect Dis 2016;62:1119–25. CrossRefexternal icon PubMedexternal icon
Legionellosis
ASHRAE. Legionellosis: Risk management for building water systems. ANSI/ASHRAE Standard 188. Atlanta, GA: ASHRAE; 2015. https:www.ashrae.orgexternal icon
Beer KD, Gargano JW, Roberts VA, et al. Outbreaks associated with environmental and undetermined water exposures—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2015;64:849–51. CrossRefexternal icon PubMedexternal icon
Beer KD, Gargano JW, Roberts VA, et al. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2015;64:842–8. CrossRefexternal icon PubMedexternal icon
CDC. Legionellosis—United States, 2000–2009. MMWR Morb Mortal Wkly Rep 2011;60:1083–6. PubMedexternal icon
CDC. Surveillance for travel-associated legionnaires disease—United States, 2005–2006. MMWR Morb Mortal Wkly Rep 2007;56:1261–3. PubMedexternal icon
Department of Veterans Affairs. Prevention of healthcare-associated Legionella disease and scald injury from potable water distribution systems. VHA Directive. 1061;2014. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3033external icon
Dooling KL, Toews KA, Hicks LA, et al. Active Bacterial Core surveillance for legionellsois—United States, 2011–2013. MMWR Morb Mortal Wkly Rep 2015;64:1190–3. CrossRefexternal icon PubMedexternal icon
Fields BS, Benson RF, Besser RE. Legionella and Legionnaires’ disease: 25 years of investigation. Clin Microbiol Rev 2002;15:506–26. CrossRefexternal icon PubMedexternal icon
Garrison LE, Kunz JM, Cooley LA, et al. Vital signs: deficiencies in environmental control identified in outbreaks of Legionnaires’ disease—North America, 2000–2014. MMWR Morb Mortal Wkly Rep 2016;65:576–84. CrossRefexternal icon PubMedexternal icon
Hlavsa MC, Roberts VA, Kahler AM, et al. Outbreaks of illness associated with recreational water—United States, 2011–2012. MMWR Morb Mortal Wkly Rep 2015;64:668–72. PubMedexternal icon
Kozak-Muiznieks NA, Lucas CE, Brown E, et al. Prevalence of sequence types among clinical and environmental isolates of Legionella pneumophila serogroup 1 in the United States from 1982 to 2012. J Clin Microbiol 2014;52:201–11. CrossRefexternal icon PubMedexternal icon
Kunz J, Cooley L. Preventing Legionnaires’ disease: environmental health expertise is key. J Environ Health 2016;79:24–6.
Marston BJ, Lipman HB, Breiman RF. Surveillance for Legionnaires’ disease. Risk factors for morbidity and mortality. Arch Intern Med 1994;154:2417–22. CrossRefexternal icon PubMedexternal icon
Weiss D, Boyd C, Rakeman JL, et al. ; South Bronx Legionnaires’ Disease Investigation Team. A large community outbreak of Legionnaires’ disease associated with a cooling tower in New York City, 2015. Public Health Rep 2017;132:241–50. CrossRefexternal icon PubMedexternal icon
Leptospirosis
Adler B, editor. Leptospira and Leptospirosis. New York, NY: Springer; 2015.
Bharti AR, Nally JE, Ricaldi JN, et al. ; Peru-United States Leptospirosis Consortium. Leptospirosis: a zoonotic disease of global importance. Lancet Infect Dis 2003;3:757–71. CrossRefexternal icon PubMedexternal icon
Haake D, Levett P. Leptospira Species (Leptospirosis). In: Bennett J, Dolin R, Blaser M, eds. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 8th ed. Philadelphia, PA: Elsevier Inc.; 2015: 2714–20.
Levett PN. Leptospirosis. Clin Microbiol Rev 2001;14:296–326. CrossRefexternal icon PubMedexternal icon
Levett PN. Usefulness of serologic analysis as a predictor of the infecting serovar in patients with severe leptospirosis. Clin Infect Dis 2003;36:447–52. CrossRefexternal icon PubMedexternal icon
Listeriosis
Cartwright EJ, Jackson KA, Johnson SD, Graves LM, Silk BJ, Mahon BE. Listeriosis outbreaks and associated food vehicles, United States, 1998–2008. Emerg Infect Dis 2013;19:1–9, quiz 184. CrossRefexternal icon PubMedexternal icon
CDC. Vital signs: Listeria illnesses, deaths, and outbreaks—United States, 2009-2011. MMWR Morb Mortal Wkly Rep 2013;62:448–52. PubMedexternal icon
Heiman KE, Garalde VB, Gronostaj M, et al. Multistate outbreak of listeriosis caused by imported cheese and evidence of cross-contamination of other cheeses, USA, 2012. Epidemiol Infect 2016;144:2698–708. CrossRefexternal icon PubMedexternal icon
Jackson KA, Biggerstaff M, Tobin-D’Angelo M, et al. Multistate outbreak of Listeria monocytogenes associated with Mexican-style cheese made from pasteurized milk among pregnant, Hispanic women. J Food Prot 2011;74:949–53. CrossRefexternal icon PubMedexternal icon
Jackson KA, Iwamoto M, Swerdlow D. Pregnancy-associated listeriosis. Epidemiol Infect 2010;138:1503–9. CrossRefexternal icon PubMedexternal icon
Jackson KA, Stroika S, Katz LS, et al. Use of whole genome sequencing and patient interviews to link a case of sporadic listeriosis to consumption of prepackaged lettuce. J Food Prot 2016;79:806–9. CrossRefexternal icon PubMedexternal icon
de Noordhout CM, Devleesschauwer B, Angulo FJ, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis 2014;14:1073–82. CrossRefexternal icon PubMedexternal icon
Matanock A, Katz LS, Jackson KA, et al. Two Listeria monocytogenes pseudo-outbreaks caused by contaminated laboratory culture media. J Clin Microbiol 2016;54:768–70. CrossRefexternal icon PubMedexternal icon
McCollum JT, Cronquist AB, Silk BJ, et al. Multistate outbreak of listeriosis associated with cantaloupe. N Engl J Med 2013;369:944–53. CrossRefexternal icon PubMedexternal icon
Pouillot R, Hoelzer K, Jackson KA, Henao OL, Silk BJ. Relative risk of listeriosis in Foodborne Diseases Active Surveillance Network (FoodNet) sites according to age, pregnancy, and ethnicity. Clin Infect Dis 2012;54(Suppl 5):S405–10. CrossRefexternal icon PubMedexternal icon
Scallan E, Hoekstra RM, Angulo FJ, et al. Foodborne illness acquired in the United States—major pathogens. Emerg Infect Dis 2011;17:7–15. CrossRefexternal icon PubMedexternal icon
Silk BJ, Date KA, Jackson KA, et al. Invasive listeriosis in the Foodborne Diseases Active Surveillance Network (FoodNet), 2004–2009: further targeted prevention needed for higher-risk groups. Clin Infect Dis 2012;54(Suppl 5):S396–404. CrossRefexternal icon PubMedexternal icon
Silk BJ, McCoy MH, Iwamoto M, Griffin PM. Foodborne listeriosis acquired in hospitals. Clin Infect Dis 2014;59:532–40. CrossRefexternal icon PubMedexternal icon
Lyme Disease
Bacon RM, Kugeler KJ, Mead PS. Surveillance for Lyme disease—United States, 1992–2006. MMWR Surveill Summ 2008;57(No. SS-10):1–9. PubMedexternal icon
Bjork J, Brown C, Friedlander H, Schiffman E, Neitzel D. Validation of random sampling as an estimation procedure for Lyme disease surveillance in Massachusetts and Minnesota. Zoonoses Public Health 2016. CrossRefexternal icon PubMedexternal icon
CDC. Three sudden cardiac deaths associated with Lyme carditis—United States, November 2012–July 2013. MMWR Morb Mortal Wkly Rep 2013;62:993–6. PubMedexternal icon
Hayes EB, Piesman J. How can we prevent Lyme disease? N Engl J Med 2003;348:2424–30. CrossRefexternal icon PubMedexternal icon
Hinckley AF, Connally NP, Meek JI, et al. Lyme disease testing by large commercial laboratories in the United States. Clin Infect Dis 2014;59:676–81. CrossRefexternal icon PubMedexternal icon
Kugeler KJ, Farley GM, Forrester JD, Mead PS. Geographic distribution and expansion of human Lyme disease, United States. Emerg Infect Dis 2015;21:1455–7. CrossRefexternal icon PubMedexternal icon
Mead P, Hinckley A, Hook S, Beard CB. TickNET-A collaborative public health approach to tickborne disease surveillance and research. Emerg Infect Dis 2015;21:1574–7. CrossRefexternal icon PubMedexternal icon
Nelson C, Hojvat S, Johnson B, et al. Concerns regarding a new culture method for Borrelia burgdorferi not approved for the diagnosis of Lyme disease. MMWR Morb Mortal Wkly Rep 2014;63:333. PubMedexternal icon
Nelson CA, Saha S, Kugeler KJ, et al. Incidence of clinician-diagnosed Lyme disease, United States, 2005–2010. Emerg Infect Dis 2015;21:1625–31. CrossRefexternal icon PubMedexternal icon
Pritt BS, Mead PS, Johnson DK, et al. Identification of a novel pathogenic Borrelia species causing Lyme borreliosis with unusually high spirochaetaemia: a descriptive study. Lancet Infect Dis 2016;16:556–64. CrossRefexternal icon PubMedexternal icon
Rutz HJ, Wee S, Feldman KA. Characterizing Lyme disease surveillance in an endemic state. Zoonoses Public Health 2016; Published online July 29, 2016. PubMedexternal icon
White J, Noonan-Toly C, Lukacik G, et al. Lyme disease surveillance in New York State: an assessment of case underreporting. Zoonoses Public Health 2016. CrossRefexternal icon PubMedexternal icon
Wormser GP, Dattwyler RJ, Shapiro ED, et al. The clinical assessment, treatment, and prevention of lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 2006;43:1089–134. CrossRefexternal icon PubMedexternal icon
Malaria
Abanyie FA, Arguin PM, Gutman J. State of malaria diagnostic testing at clinical laboratories in the United States, 2010: a nationwide survey. Malar J 2011;10:340. CrossRefexternal icon PubMedexternal icon
Cullen KA, Mace KE, Arguin PM. Malaria surveillance—United States, 2013. MMWR Surveill Summ 2016;65(No. SS-2):1–22. CrossRefexternal icon PubMedexternal icon
Hwang J, Cullen KA, Kachur SP, Arguin PM, Baird JK. Severe morbidity and mortality risk from malaria in the United States, 1985–2011. Open Forum Infect Dis 2014;1:ofu034. CrossRefexternal icon PubMedexternal icon
Jensenius M, Han PV, Schlagenhauf P, et al. ; GeoSentinel Surveillance Network. Acute and potentially life-threatening tropical diseases in western travelers—a GeoSentinel multicenter study, 1996–2011. Am J Trop Med Hyg 2013;88:397–404. CrossRefexternal icon PubMedexternal icon
Krause G, Schöneberg I, Altmann D, Stark K. Chemoprophylaxis and malaria death rates. Emerg Infect Dis 2006;12:447–51. CrossRefexternal icon PubMedexternal icon
Mace KE, Arguin PM. Malaria Surveillance—United States, 2014. MMWR Surveill Summ 2017;66(No. SS-12):1–24. CrossRefexternal icon PubMedexternal icon
Tan KR, Cullen KA, Koumans EH, Arguin PM. Inadequate diagnosis and treatment of malaria among travelers returning from Africa during the Ebola epidemic—United States, 2014–2015. MMWR Morb Mortal Wkly Rep 2016;65:27–9. CrossRefexternal icon PubMedexternal icon
Measles
McLean HQ, Fiebelkorn AP, Temte JL, Wallace GS. Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: summary recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(No.RR-4):1–34. PubMedexternal icon
Papania MJ, Wallace GS, Rota PA, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: the US experience. JAMA Pediatr 2014;168:148–55. CrossRefexternal iconPubMedexternal icon
Meningococcal Disease
Cohn AC, MacNeil JR, Clark TA, et al. Prevention and control of meningococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2013;62(No.RR-2):1–28. PubMedexternal icon
Cohn AC, MacNeil JR, Harrison LH, et al. Changes in Neisseria meningitidis disease epidemiology in the United States, 1998–2007: implications for prevention of meningococcal disease. Clin Infect Dis 2010;50:184–91. CrossRefexternal icon PubMedexternal icon
Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. N Engl J Med 2001;344:1378–88. CrossRefexternal icon PubMedexternal icon
Mumps
Fiebelkorn AP, Lawler J, Curns AT, Brandeburg C, Wallace GS. Mumps postexposure prophylaxis with a third dose of measles-mumps-rubella vaccine, Orange County, New York, USA. Emerg Infect Dis 2013;19:1411–7. CrossRefexternal icon PubMedexternal icon
Parker Fiebelkorn AP, Rosen JB, Brown C, et al. Environmental factors potentially associated with mumps transmission in yeshivas during a mumps outbreak among highly vaccinated students: Brooklyn, New York, 2009-2010. Hum Vaccin Immunother 2013;9:189–94. CrossRefexternal icon PubMedexternal icon
Novel Influenza A Virus Infections
Bowman AS, Workman JD, Nolting JM, Nelson SW, Slemons RD. Exploration of risk factors contributing to the presence of influenza A virus in swine at agricultural fairs. Emerg Microbes Infect 2014;3:e5. CrossRefexternal icon PubMedexternal icon
CDC. Antibodies cross-reactive to influenza A (H3N2) variant virus and impact of 2010–11 seasonal influenza vaccine on cross-reactive antibodies—United States. MMWR Morb Mortal Wkly Rep 2012;61:237–41. PubMedexternal icon
Ducatez MF, Hause B, Stigger-Rosser E, et al. Multiple reassortment between pandemic (H1N1) 2009 and endemic influenza viruses in pigs, United States. Emerg Infect Dis 2011;17:1624–9. CrossRefexternal icon PubMedexternal icon
Epperson S, Jhung M, Richards S, et al. ; Influenza A (H3N2)v Virus Investigation Team. Human infections with influenza A(H3N2) variant virus in the United States, 2011–2012. Clin Infect Dis 2013;57(Suppl 1):S4–11. CrossRefexternal icon PubMedexternal icon
Jhung MA, Epperson S, Biggerstaff M, et al. Outbreak of variant influenza A(H3N2) virus in the United States. Clin Infect Dis 2013;57:1703–12. CrossRefexternal icon PubMedexternal icon
Myers KP, Olsen CW, Gray GC. Cases of swine influenza in humans: a review of the literature. Clin Infect Dis 2007;44:1084–8. CrossRefexternal icon PubMedexternal icon
National Assembly of State Animal Health Officials; National Association of State Public Health Veterinarians. Measures to minimize influenza transmission at swine exhibitions. Arlington, VA: National Assembly of State Animal Health Officials; 2014. https://www.cdc.gov/flu/pdf/swineflu/influenza-transmission-swine-exhibitions-2014.pdfpdf icon
Olsen CW. The emergence of novel swine influenza viruses in North America. Virus Res 2002;85:199–210. CrossRefexternal icon PubMedexternal icon
Rajão DS, Gauger PC, Anderson TK, et al. Novel reassortant human-like H3N2 and H3N1 influenza A viruses detected in pigs are virulent and antigenically distinct from swine viruses endemic to the United States. J Virol 2015;89:11213–22. CrossRefexternal icon PubMedexternal icon
Schicker RS, Rossow J, Eckel S, et al. Outbreak of influenza A (H3N2) variant virus infections among persons attending agricultural fairs housing infected swine—Michigan and Ohio, July–August 2016. MMWR Morb Mortal Wkly Rep 2016;65:1157–60. CrossRefexternal icon PubMedexternal icon
Shinde V, Bridges CB, Uyeki TM, et al. Triple-reassortant swine influenza A (H1) in humans in the United States, 2005–2009. N Engl J Med 2009;360:2616–25. CrossRefexternal icon PubMedexternal icon
Vincent AL, Ma W, Lager KM, Janke BH, Richt JA. Swine influenza viruses a North American perspective. Adv Virus Res 2008;72:127–54. CrossRefexternal icon PubMedexternal icon
Vincent AL, Swenson SL, Lager KM, Gauger PC, Loiacono C, Zhang Y. Characterization of an influenza A virus isolated from pigs during an outbreak of respiratory disease in swine and people during a county fair in the United States. Vet Microbiol 2009;137:51–9. CrossRefexternal icon PubMedexternal icon
Pertussis
Acosta AM, DeBolt C, Tasslimi A, et al. Tdap vaccine effectiveness in adolescents during the 2012 Washington State pertussis epidemic. Pediatrics 2015;135:981–9. CrossRefexternal icon PubMedexternal icon
Breakwell L, Kelso P, Finley C, et al. Pertussis vaccine effectiveness in the setting of pertactin-deficient pertussis, Vermont. Pediatrics 2016;137:e20153973. CrossRefexternal icon PubMedexternal icon
CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep 2012;61:468–70. PubMedexternal icon
CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (Tdap) in pregnant women—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep 2013;62:131–5. PubMedexternal icon
Skoff TH, Kenyon C, Cocoros N, et al. Sources of infant pertussis infection in the United States. Pediatrics 2015;136:635–41. CrossRefexternal icon PubMedexternal icon
Skoff TH, Martin SW. Impact of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccination on reported pertussis cases among adolescents 11–18 years of age in an era of waning pertussis immunity: a follow-up analysis. JAMA Pediatr 2016;170:453–8. CrossRefexternal icon PubMedexternal icon
Plague
Dennis DT, Gage KL, Gratz N, Poland JD, Tikhomirov E. Plague manual: epidemiology, distribution, surveillance, and control. Geneva, Switzerland: World Health Organization; 1999.
Inglesby TV, Dennis DT, Henderson DA, et al. ; Working Group on Civilian Biodefense. Plague as a biological weapon: medical and public health management. JAMA 2000;283:2281–90. CrossRefexternal icon PubMedexternal icon
Kugeler KJ, Staples JE, Hinckley AF, Gage KL, Mead PS. Epidemiology of human plague in the United States, 1900–2012. Emerg Infect Dis 2015;21:16–22. CrossRefexternal icon PubMedexternal icon
Kwit N, Nelson C, Kugeler K, et al. Human plague—United States, 2015. MMWR Morb Mortal Wkly Rep 2015;64:918–9. CrossRefexternal icon PubMedexternal icon
Runfola JK, House J, Miller L, et al. Outbreak of human pneumonic plague with dog-to-human and possible human-to-human transmission—Colorado, June–July 2014. MMWR Morb Mortal Wkly Rep 2015;64:429–34. PubMedexternal icon
Tourdjman M, Ibraheem M, Brett M, et al. Misidentification of Yersinia pestis by automated systems, resulting in delayed diagnoses of human plague infections—Oregon and New Mexico, 2010–2011. Clin Infect Dis 2012;55:e58–60. CrossRefexternal icon PubMedexternal icon
Q Fever
Anderson A, Bijlmer H, Fournier PE, et al. Diagnosis and management of Q Fever—United States, 2013: recommendations from CDC and the Q Fever working group. MMWR Recomm Rep 2013;62(No. RR-3):1–30. PubMedexternal icon
Dahlgren FS, Haberling DL, McQuiston JH. Q fever is underestimated in the United States: a comparison of fatal Q fever cases from two national reporting systems. Am J Trop Med Hyg 2015;92:244–6. CrossRefexternal icon PubMedexternal icon
Dahlgren FS, McQuiston JH, Massung RF, Anderson AD. Q fever in the United States: summary of case reports from two national surveillance systems, 2000–2012. Am J Trop Med Hyg 2015;92:247–55. CrossRefexternal icon PubMedexternal icon
Eldin C, Mélenotte C, Mediannikov O, et al. From Q Fever to Coxiella burnetii infection: a paradigm change. Clin Microbiol Rev 2017;30:115–90. CrossRefexternal icon PubMedexternal icon
Rabies
CDC. Human rabies prevention—United States, 2008: recommendation of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2008;57(No. RR-3).
Brown CM, Slavinski S, Ettestad P, Sidwa TJ, Sorhage FE; National Association of State Public Health Veterinarians; Compendium of Animal Rabies Prevention and Control Committee. Compendium of animal rabies prevention and control, 2016. J Am Vet Med Assoc 2016;248:505–17. CrossRefexternal icon PubMedexternal icon
Rupprecht CE, Briggs D, Brown CM, et al. Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies: recommendations of the advisory committee on immunization practices. MMWR Recomm Rep 2010;59(No. RR-2):1–9. PubMedexternal icon
Salmonellosis
Chai SJ, White PL, Lathrop SL, et al. Salmonella enterica serotype Enteritidis: increasing incidence of domestically acquired infections. Clin Infect Dis 2012;54(Suppl 5):S488–97. CrossRefexternal icon PubMedexternal icon
Guo C, Hoekstra RM, Schroeder CM, et al. Application of Bayesian techniques to model the burden of human salmonellosis attributable to U.S. food commodities at the point of processing: adaptation of a Danish model. Foodborne Pathog Dis 2011;8:509–16. CrossRefexternal icon PubMedexternal icon
Jackson BR, Griffin PM, Cole D, Walsh KA, Chai SJ. Outbreak-associated Salmonella enterica serotypes and food commodities, United States, 1998–2008. Emerg Infect Dis 2013;19:1239–44. CrossRefexternal icon PubMedexternal icon
Jones TF, Ingram LA, Cieslak PR, et al. Salmonellosis outcomes differ substantially by serotype. J Infect Dis 2008;198:109–14. CrossRefexternal icon PubMedexternal icon
Painter JA, Hoekstra RM, Ayers T, et al. Attribution of foodborne illnesses, hospitalizations, and deaths to food commodities by using outbreak data, United States, 1998–2008. Emerg Infect Dis 2013;19:407–15. CrossRefexternal icon PubMedexternal icon
Scallan E, Mahon BE, Hoekstra RM, Griffin PM. Estimates of illnesses, hospitalizations and deaths caused by major bacterial enteric pathogens in young children in the United States. Pediatr Infect Dis J 2013;32:217–21. PubMedexternal icon
Medalla F, Gu W, Mahon BE, et al. Estimated incidence of antimicrobial drug–resistant nontyphoidal Salmonella infections, United States, 2004–2012. Emerg Infect Dis 2016;23:29–37. CrossRefexternal icon PubMedexternal icon
Iwamoto M, Reynolds J, Karp BE, et al. Ceftriaxone-resistant nontyphoidal Salmonella from humans, retail meats, and food animals in the United States, 1996–2013. Foodborne Pathog Dis 2017;14:74–83. CrossRefexternal icon PubMedexternal icon
Shiga toxin-producing Escherichia coli (STEC)
Gould LH, Mody RK, Ong KL, et al. ; Emerging Infections Program Foodnet Working Group. Increased recognition of non-O157 Shiga toxin-producing Escherichia coli infections in the United States during 2000–2010: epidemiologic features and comparison with E. coli O157 infections. Foodborne Pathog Dis 2013;10:453–60. CrossRefexternal icon PubMedexternal icon
Hale CR, Scallan E, Cronquist AB, et al. Estimates of enteric illness attributable to contact with animals and their environments in the United States. Clin Infect Dis 2012;54(Suppl 5):S472–9. CrossRefexternal icon PubMedexternal icon
Iwamoto M, Huang JY, Cronquist AB, et al. Bacterial enteric infections detected by culture-independent diagnostic tests—FoodNet, United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015;64:252–7. PubMedexternal icon
Jones TF, Gerner-Smidt P. Nonculture diagnostic tests for enteric diseases. Emerg Infect Dis 2012;18:513–4. CrossRefexternal icon PubMedexternal icon
Mody RK, Griffin PM. Fecal shedding of Shiga toxin-producing Escherichia coli: what should be done to prevent secondary cases? Clin Infect Dis 2013;56:1141–4. CrossRefexternal icon PubMedexternal icon
Mody RK, Griffin PM. Increasing evidence that certain antibiotics should be avoided for shiga toxin–producing Escherichia coli infections: more data needed. Clin Infect Dis 2016;62:1259–61. CrossRefexternal icon PubMedexternal icon
Mody RK, Luna-Gierke RE, Jones TF, et al. Infections in pediatric postdiarrheal hemolytic uremic syndrome: factors associated with identifying shiga toxin-producing Escherichia coli. Arch Pediatr Adolesc Med 2012;166:902–9. CrossRefexternal icon PubMedexternal icon
Tarr PI, Gordon CA, Chandler WL. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 2005;365:1073–86. PubMedexternal icon
Shigellosis
Arvelo W, Hinkle CJ, Nguyen TA, et al. Transmission risk factors and treatment of pediatric shigellosis during a large daycare center-associated outbreak of multidrug resistant Shigella sonnei: implications for the management of shigellosis outbreaks among children. Pediatr Infect Dis J 2009;28:976–80. CrossRefexternal icon PubMedexternal icon
Baker KS, Dallman TJ, Ashton PM, et al. Intercontinental dissemination of azithromycin-resistant shigellosis through sexual transmission: a cross-sectional study. Lancet Infect Dis 2015;15:913–21. CrossRefexternal icon PubMedexternal icon
Bowen A, Hurd J, Hoover C, et al. Importation and domestic transmission of Shigella sonnei resistant to ciprofloxacin—United States, May 2014–February 2015. MMWR Morb Mortal Wkly Rep 2015;64:318–20. PubMedexternal icon
CDC. Outbreaks of multidrug-resistant Shigella sonnei gastroenteritis associated with day care centers—Kansas, Kentucky, and Missouri, 2005. MMWR Mortal Wkly Rep 2006;55:1068–71.
CDC. Notes from the field: Outbreak of infections caused by Shigella sonnei with decreased susceptibility to azithromycin—Los Angeles, California, 2012. MMWR Morb Mortal Wkly Rep 2013;62:171. PubMedexternal icon
Bowen A, Eikmeier D, Talley P, et al. . Notes from the field: outbreaks of Shigella sonnei infection with decreased susceptibility to azithromycin among men who have sex with men—Chicago and Metropolitan Minneapolis-St. Paul, 2014. MMWR Morb Mortal Wkly Rep 2015;64:597–8. PubMedexternal icon
Folster JP, Pecic G, Bowen A, Rickert R, Carattoli A, Whichard JM. Decreased susceptibility to ciprofloxacin among Shigella isolates in the United States, 2006 to 2009. Antimicrob Agents Chemother 2011;55:1758–60. CrossRefexternal icon PubMedexternal icon
Garrett V, Bornschlegel K, Lange D, et al. A recurring outbreak of Shigella sonnei among traditionally observant Jewish children in New York City: the risks of daycare and household transmission. Epidemiol Infect 2006;134:1231–6. CrossRefexternal icon PubMedexternal icon
Gray MD, Lampel KA, Strockbine NA, Fernandez RE, Melton-Celsa AR, Maurelli AT. Clinical isolates of Shiga toxin 1a-producing Shigella flexneri with an epidemiological link to recent travel to Hispañiola. Emerg Infect Dis 2014;20:1669–77. CrossRefexternal icon PubMedexternal icon
Gupta A, Polyak CS, Bishop RD, Sobel J, Mintz ED. Laboratory-confirmed shigellosis in the United States, 1989-2002: epidemiologic trends and patterns. Clin Infect Dis 2004;38:1372–7. CrossRefexternal icon PubMedexternal icon
Huang JY, Henao OL, Griffin PM, et al. Infection with pathogens transmitted commonly through food and the effect of increasing use of culture-independent diagnostic tests on surveillance–Foodborne Diseases Active Surveillance Network, 10 U.S. sites, 2012–2015. MMWR Morb Mortal Wkly Rep 2016;65:368–71. CrossRefexternal icon PubMedexternal icon
Lederer I, Taus K, Allerberger F, et al. Shigellosis in refugees, Austria, July to November 2015. Euro Surveill 2015;20:30081. CrossRefexternal icon PubMedexternal icon
Nygren BL, Schilling KA, Blanton EM, Silk BJ, Cole DJ, Mintz ED. Foodborne outbreaks of shigellosis in the USA, 1998–2008. Epidemiol Infect 2013;141:233–41 . CrossRefexternal icon PubMedexternal icon
Scallan E, Mahon BE, Hoekstra RM, Griffin PM. Estimates of illnesses, hospitalizations and deaths caused by major bacterial enteric pathogens in young children in the United States. Pediatr Infect Dis J 2013;32:217–21. PubMedexternal icon
Spotted Fever Rickettsiosis
CDC. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever and other spotted fever group rickettsioses, ehrlichioses, and anaplasmosis—United States: a practical guide for health care and public health professionals. MMWR Recomm Rep 2016;65(No. RR-2).
Dahlgren FS, Paddock CD, Springer YP, Eisen RJ, Behravesh CB. Expanding range of Amblyomma americanum and simultaneous changes in the epidemiology of spotted fever group Rickettsiosis in the United States, 1999–2007. Am J Trop Med Hyg 2016;94:35–42. CrossRefexternal icon PubMedexternal icon
Drexler NA, Dahlgren FS, Heitman KN, Massung RF, Paddock CD, Behravesh CB. National surveillance of spotted fever group Rickettsiosis in the United States, 2008–2012. Am J Trop Med Hyg 2016;94:26–34. CrossRefexternal icon PubMedexternal icon
Herrick KL, Pena SA, Yaglom HD, et al. Rickettsia parkeri Rickettsiosis, Arizona, USA. Emerg Infect Dis 2016;22:780–5. CrossRefexternal icon PubMedexternal icon
Johnston SH, Glaser CA, Padgett K, et al. Rickettsia spp. 364D causing a cluster of eschar-associated illness, California. Pediatr Infect Dis J 2013;32:1036–9. CrossRefexternal icon PubMedexternal icon
Paddock CD, Goddard J. The evolving medical and veterinary importance of the Gulf Coast tick (Acari: Ixodidae). J Med Entomol 2015;52:230–52. CrossRefexternal icon PubMedexternal icon
Padgett KA, Bonilla D, Eremeeva ME, et al. The Eco-epidemiology of Pacific Coast Tick Fever in California. PLoS Negl Trop Dis 2016;10:e0005020. CrossRefexternal icon PubMedexternal icon
Straily A, Feldpausch A, Ulbrich C, et al. Notes from the field: Rickettsia parkeri Rickettsiosis—Georgia, 2012–2014. MMWR Morb Mortal Wkly Rep 2016;65:718–9. CrossRefexternal icon PubMedexternal icon
Streptococcal Toxic Shock Syndrome
CDC. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Group A Streptococcus—2014. https://www.cdc.gov/abcs/reports-findings/survreports/gas14.pdfpdf icon
CDC. Investigating clusters of group A streptococcal disease. Atlanta, GA: US Department of Health and Human Services, CDC; 2009. https://www.cdc.gov/groupastrep/outbreaks/calculator
Nelson GE, Pondo T, Toews KA, et al. Epidemiology of invasive group A streptococcal infections in the United States, 2005–2012. Clin Infect Dis 2016;63:478–86. CrossRefexternal icon PubMedexternal icon
Prevention of Invasive Group A Streptococcal Infections Workshop Participants. Prevention of invasive group A streptococcal disease among household contacts of case patients and among postpartum and postsurgical patients: recommendations from the Centers for Disease Control and Prevention. Clin Infect Dis 2002;35:950–9 . CrossRefexternal icon PubMedexternal icon
Smit MA, Nyquist AC, Todd JK. Infectious shock and toxic shock syndrome diagnoses in hospitals, Colorado, USA. Emerg Infect Dis 2013;19:1855–8. CrossRefexternal icon PubMedexternal icon
Steer AC, Carapetis JR, Dale JB, et al. Status of research and development of vaccines for Streptococcus pyogenes. Vaccine 2016;34:2953–8. CrossRefexternal icon PubMedexternal icon
Syphilis
CDC. Sexually transmitted disease surveillance, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016.
Patton ME, Su JR, Nelson R, Weinstock H. Primary and secondary syphilis—United States, 2005–2013. MMWR Morb Mortal Wkly Rep 2014;63:402–6. PubMedexternal icon
Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3):1–137. PubMedexternal icon
Syphilis, Congenital
Bowen V, Su J, Torrone E, Kidd S, Weinstock H. Increase in incidence of congenital syphilis—United States, 2012–2014. MMWR Morb Mortal Wkly Rep 2015;64:1241–5. CrossRefexternal icon PubMedexternal icon
CDC. Sexually transmitted disease surveillance, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016.
Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3):1–137. PubMedexternal icon
Tetanus
CDC. Tetanus—Puerto Rico, 2002. MMWR Morb Mortal Wkly Rep 2002;51:613–5. PubMedexternal icon
Khetsuriani N, Zakikhany K, Jabirov S, et al. Seroepidemiology of diphtheria and tetanus among children and young adults in Tajikistan: nationwide population-based survey, 2010. Vaccine 2013;31:4917–22. CrossRefexternal icon PubMedexternal icon
McQuillan GM, Kruszon-Moran D, Deforest A, Chu SY, Wharton M. Serologic immunity to diphtheria and tetanus in the United States. Ann Intern Med 2002;136:660–6. CrossRefexternal icon PubMedexternal icon
Pascual FB, McGinley EL, Zanardi LR, Cortese MM, Murphy TV. Tetanus surveillance—United States, 1998–2000. MMWR Surveill Summ 2003;52(No. SS-3):1–8. PubMedexternal icon
Roper M, Wassilak S, Tiwari T, Orenstein W. Tetanus toxoid. In: Plotkin O, Orenstein W, Offitt P, eds. Vaccines. Edinburgh: Saunders, 2012.
Trichinellosis
Greene YG, Padovani T, Rudroff JA, Hall R, Austin C, Vernon M. Trichinellosis caused by consumption of wild boar meat—Illinois, 2013. MMWR Morb Mortal Wkly Rep 2014;63:451. PubMedexternal icon
Gamble HR, Bessonov AS, Cuperlovic K, et al. International Commission on Trichinellosis: recommendations on methods for the control of Trichinella in domestic and wild animals intended for human consumption. Vet Parasitol 2000;93:393–408. CrossRefexternal icon PubMedexternal icon
Gottstein B, Pozio E, Nöckler K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clin Microbiol Rev 2009;22:127–45. CrossRefexternal icon PubMedexternal icon
Holzbauer SM, Agger WA, Hall RL, et al. Outbreak of Trichinella spiralis infections associated with a wild boar hunted at a game farm in Iowa. Clin Infect Dis 2014;59:1750–6. CrossRefexternal icon PubMedexternal icon
Kennedy ED, Hall RL, Montgomery SP, Pyburn DG, Jones JL. Trichinellosis surveillance—United States, 2002–2007. MMWR Surveill Summ 2009;58(No. SS-9):1–7. PubMedexternal icon
Roy SL, Lopez AS, Schantz PM. Trichinellosis surveillance—United States, 1997–2001. MMWR Surveill Summ 2003;52(No. SS-6):1–8. PubMedexternal icon
Wilson NO, Hall RL, Montgomery SP, Jones JL. Trichinellosis surveillance—United States, 2008–2012. MMWR Surveill Summ 2015;64(No. SS-1):1–8. PubMedexternal icon
Tuberculosis
CDC. Reported tuberculosis in the United States, 2015. Atlanta, GA: US Department of Health and Human Services, CDC; 2016.
France AM, Grant J, Kammerer JS, Navin TR. A field-validated approach using surveillance and genotyping data to estimate tuberculosis attributable to recent transmission in the United States. Am J Epidemiol 2015;182:799–807. CrossRefexternal icon PubMedexternal icon
Manangan LP, Tryon C, Magee E, Miramontes R. Innovative quality-assurance strategies for tuberculosis surveillance in the United States. Tuberc Res Treat 2012:2012:481230.
Salinas JL, Mindra G, Haddad MB, Pratt R, Price SF, Langer AJ. Leveling of tuberculosis incidence—United States, 2013–2015. MMWR Morb Mortal Wkly Rep 2016;65:273–8. CrossRefexternal icon PubMedexternal icon
Woodruff RS, Winston CA, Miramontes R. Predicting U.S. tuberculosis case counts through 2020. PLoS One 2013;8:e65276. CrossRefexternal icon PubMedexternal icon
Yelk Woodruff RS, Pratt RH, Armstrong LR. The US National Tuberculosis Surveillance System: A descriptive assessment of the completeness and consistency of data reported from 2008 to 2012. JMIR Public Health Surveill 2015;1:e15. CrossRefexternal icon PubMedexternal icon
Yuen CM, Kammerer JS, Marks K, Navin TR, France AM. Recent transmission of tuberculosis—United States, 2011–2014. PLoS One 2016;11:e0153728. CrossRefexternal icon PubMedexternal icon
Tularemia
CDC. Tularemia—United States, 2001–2010. MMWR Morb Mortal Wkly Rep 2013;62:963–6. PubMedexternal icon
Dennis DT, Inglesby TV, Henderson DA, et al. ; Working Group on Civilian Biodefense. Tularemia as a biological weapon: medical and public health management. JAMA 2001;285:2763–73. CrossRefexternal icon PubMedexternal icon
Kugeler KJ, Mead PS, Janusz AM, et al. Molecular epidemiology of Francisella tularensis in the United States. Clin Infect Dis 2009;48:863–70. CrossRefexternal icon PubMedexternal icon
Pedati C, House J, Hancock-Allen J, et al. Notes from the field: increase in human cases of tularemia—Colorado, Nebraska, South Dakota, and Wyoming, January–September 2015. MMWR Morb Mortal Wkly Rep 2015;64:1317–8. CrossRefexternal icon PubMedexternal icon
Tarnvik A. WHO guidelines on tularemia. Geneva, Switzerland: World Health Organization; 2007.
Weber IB, Turabelidze G, Patrick S, Griffith KS, Kugeler KJ, Mead PS. Clinical recognition and management of tularemia in Missouri: a retrospective records review of 121 cases. Clin Infect Dis 2012;55:1283–90. CrossRefexternal icon PubMedexternal icon
Typhoid
Date KA, Newton AE, Medalla F, et al. Changing patterns in enteric fever incidence and increasing antibiotic resistance of enteric fever isolates in the United States, 2008–2012. Clin Infect Dis 2016;63:322–9. CrossRefexternal icon PubMedexternal icon
Imanishi M, Newton AE, Vieira AR, et al. Typhoid fever acquired in the United States, 1999–2010: epidemiology, microbiology, and use of a space-time scan statistic for outbreak detection. Epidemiol Infect 2015;143:2343–54. CrossRefexternal icon PubMedexternal icon
Loharikar A, Newton A, Rowley P, et al. Typhoid fever outbreak associated with frozen mamey pulp imported from Guatemala to the western United States, 2010. Clin Infect Dis 2012;55:61–6. CrossRefexternal icon PubMedexternal icon
Lynch MF, Blanton EM, Bulens S, et al. Typhoid fever in the United States, 1999–2006. JAMA 2009;302:859–65. CrossRefexternal icon PubMedexternal icon
Mahon BE, Newton AE, Mintz ED. Effectiveness of typhoid vaccination in US travelers. Vaccine 2014;32:3577–9. CrossRefexternal icon PubMedexternal icon
Olsen SJ, Bleasdale SC, Magnano AR, et al. Outbreaks of typhoid fever in the United States, 1960–99. Epidemiol Infect 2003;130:13–21. CrossRefexternal icon PubMedexternal icon
Steinberg EB, Bishop R, Haber P, et al. Typhoid fever in travelers: who should be targeted for prevention? Clin Infect Dis 2004;39:186–91. CrossRefexternal icon PubMedexternal icon
Varicella
Bialek SR, Perella D, Zhang J, et al. Impact of a routine two-dose varicella vaccination program on varicella epidemiology. Pediatrics 2013;132:e1134–40. CrossRefexternal icon PubMedexternal icon
Lopez AS, Zhang J, Brown C, Bialek S. Varicella-related hospitalizations in the United States, 2000–2006: the 1-dose varicella vaccination era. Pediatrics 2011;127:238–45. CrossRefexternal icon PubMedexternal icon
Lopez AS, Zhang J, Marin M. Epidemiology of varicella during the 2-dose Varicella Vaccination Program—United States, 2005–2014. MMWR Morb Mortal Wkly Rep 2016;65:902–5. CrossRefexternal icon PubMedexternal icon
Marin M, Güris D, Chaves SS, Schmid S, Seward JF; Advisory Committee on Immunization Practices, CDC. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 2007;56(No. RR-4):1–40. PubMedexternal icon
Marin M, Zhang JX, Seward JF. Near elimination of varicella deaths in the US after implementation of the vaccination program. Pediatrics 2011;128:214–20. CrossRefexternal icon PubMedexternal icon
Vibriosis
Crowe SJ, Newton AE, Gould LH, et al. Vibriosis, not cholera: toxigenic Vibrio cholerae non-O1, non-O139 infections in the United States, 1984–2014. Epidemiol Infect 2016;144:3335–41. CrossRefexternal icon PubMedexternal icon
Daniels NA, MacKinnon L, Bishop R, et al. Vibrio parahaemolyticus infections in the United States, 1973–1998. J Infect Dis 2000;181:1661–6. CrossRefexternal icon PubMedexternal icon
Dechet AM, Yu PA, Koram N, Painter J. Nonfoodborne Vibrio infections: an important cause of morbidity and mortality in the United States, 1997–2006. Clin Infect Dis 2008;46:970–6. CrossRefexternal icon PubMedexternal icon
McLaughlin JB, DePaola A, Bopp CA, et al. Outbreak of Vibrio parahaemolyticus gastroenteritis associated with Alaskan oysters. N Engl J Med 2005;353:1463–70. CrossRefexternal icon PubMedexternal icon
Newton AE, Garrett N, Stroika SG, Halpin JL, Turnsek M, Mody RK. Increase in Vibrio parahaemolyticus infections associated with consumption of Atlantic Coast shellfish—2013. MMWR Morb Mortal Wkly Rep 2014;63:335–6. PubMedexternal icon
Newton A, Kendall M, Vugia DJ, Henao OL, Mahon BE. Increasing rates of vibriosis in the United States, 1996–2010: review of surveillance data from 2 systems. Clin Infect Dis 2012;54(Suppl 5):S391–5. CrossRefexternal icon PubMedexternal icon
Shapiro RL, Altekruse S, Hutwagner L, et al. ; Vibrio Working Group. The role of Gulf Coast oysters harvested in warmer months in Vibrio vulnificus infections in the United States, 1988–1996. J Infect Dis 1998;178:752–9. CrossRefexternal icon PubMedexternal icon
Tobin-D’Angelo M, Smith AR, Bulens SN, et al. Severe diarrhea caused by cholera toxin-producing vibrio cholerae serogroup O75 infections acquired in the southeastern United States. Clin Infect Dis 2008;47:1035–40. CrossRefexternal icon PubMedexternal icon
Vugia DJ, Tabnak F, Newton AE, Hernandez M, Griffin PM. Impact of 2003 state regulation on raw oyster-associated Vibrio vulnificus illnesses and deaths, California, USA. Emerg Infect Dis 2013;19:1276–80. CrossRefexternal icon PubMedexternal icon
Suggested citation for this article: Adams DA, Thomas KR, Jajosky RA, et al. Summary of Notifiable Infectious Diseases and Conditions — United States, 2015. MMWR Morb Mortal Wkly Rep 2017;64:1–143. DOI: http://dx.doi.org/10.15585/mmwr.mm6453a1external icon.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to [email protected].