COVID-19 Mitigation Behaviors by Age Group — United States, April–June 2020
Weekly / October 30, 2020 / 69(43);1584–1590
On October 27, 2020, this report was posted online as an MMWR Early Release.
Please note:. This report has been corrected.
Helena J. Hutchins, MPH1; Brent Wolff, PhD1; Rebecca Leeb, PhD1; Jean Y. Ko, PhD1; Erika Odom, PhD1; Joe Willey, PhD2; Allison Friedman1; Rebecca H. Bitsko, PhD3 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
Recommended mitigation behaviors to prevent the spread of COVID-19 include wearing masks, hand washing, social distancing, and staying home when ill.
What is added by this report?
Self-reported engagement in mitigation behaviors (mask wearing, handwashing, physical distancing, crowd and restaurant avoidance, and cancellation of social activities) differed significantly by adult age group. During April–June 2020, the prevalence of these behaviors was lowest among adults aged 18–29 years and highest among those aged >60 years. Whereas mask wearing increased over time, other reported mitigation behaviors decreased or remained unchanged.
What are the implications for public health practice?
Improved communication and policy priorities are needed to promote recommended COVID-19 mitigation behaviors, particularly among young adults.
CDC recommends a number of mitigation behaviors to prevent the spread of SARS-CoV-2, the virus that causes coronavirus disease 2019 (COVID-19). Those behaviors include 1) covering the nose and mouth with a mask to protect others from possible infection when in public settings and when around persons who live outside of one’s household or around ill household members; 2) maintaining at least 6 feet (2 meters) of distance from persons who live outside one’s household, and keeping oneself distant from persons who are ill; and 3) washing hands often with soap and water for at least 20 seconds, or, if soap and water are not available, using hand sanitizer containing at least 60% alcohol (1). Age has been positively associated with mask use (2), although less is known about other recommended mitigation behaviors. Monitoring mitigation behaviors over the course of the pandemic can inform targeted communication and behavior modification strategies to slow the spread of COVID-19. The Data Foundation COVID Impact Survey collected nationally representative data on reported mitigation behaviors during April–June 2020 among adults in the United States aged ≥18 years (3). Reported use of face masks increased from 78% in April, to 83% in May, and reached 89% in June; however, other reported mitigation behaviors (e.g., hand washing, social distancing, and avoiding public or crowded places) declined marginally or remained unchanged. At each time point, the prevalence of reported mitigation behaviors was lowest among younger adults (aged 18–29 years) and highest among older adults (aged ≥60 years). Lower engagement in mitigation behaviors among younger adults might be one reason for the increased incidence of confirmed COVID-19 cases in this group, which have been shown to precede increases among those >60 years (4). These findings underscore the need to prioritize clear, targeted messaging and behavior modification interventions, especially for young adults, to encourage uptake and support maintenance of recommended mitigation behaviors to prevent the spread of COVID-19.
The COVID Impact Survey collected data to provide national estimates of health, economic, and social well-being of U.S. adults, using a national probability sample covering approximately 97% of the U.S. population of non-institutionalized adults with a home address (3). Surveys were conducted in three waves (April 20–26, May 4–10, and May 30–June 8), without significant resampling of persons across waves. Analyses included a total of 6,475 online or telephone surveys of adults aged ≥18 years.* The response rate among those invited to participate ranged from 19.7% to 26.1% across the three survey waves. Following data collection, an iterative raking process was used to adjust for nonresponse, noncoverage, and under- and oversampling (5). Demographic weighting variables provided in the dataset were obtained from the 2020 Current Population Survey; estimates reflect the U.S. household population of adults aged ≥18 years.† No personally identifying information was provided in the data file accessed by CDC.§
Respondents were asked, “Which of the following measures, if any, are you taking in response to the coronavirus?” Of the 19 response options, three mitigation behaviors aligning with CDC recommendations were assessed: 1) “wore a face mask,” 2) “washed or sanitized hands,” and 3) “kept six feet distance from those outside my household.”¶ Three social mitigation behaviors aligning with CDC considerations and White House guidelines from March and April 2020 also were selected for analysis: 1) “avoided public or crowded places,” 2) “cancelled or postponed social or recreational activities,” and 3) “avoided some or all restaurants.”**,††,§§ Pearson’s Chi-squared test was used to assess differences in reported behaviors (individual and cumulative) by age, within each survey wave and stratified by face mask use, based on a significance level of α = 0.05. Logistic regression models were used to test statistical significance of time trends by assigning calendar week of data collection for each survey wave as a single linear predictor for individual and cumulative behavioral outcomes. All analyses were conducted in Stata ES (version 16.1, StataCorp.) with survey weights applied during analyses for nationally representative estimates.
Across survey waves, the majority of the weighted sample (range = 62%–65%) identified as Non-Hispanic or Latino White, and 50% identified as female; 14%–15% of respondents were aged 18–29 years. In April, 78% of adults aged ≥18 years reported wearing a mask; this increased to 83% in May and 89% in June (Table 1) (p<0.001). All other reported mitigation behaviors decreased from April 20–26 to early June (p<0.05), except avoiding some or all restaurants, which did not change significantly (Table 1) (Supplementary Figure 1: https://stacks.cdc.gov/view/cdc/95944). At each time point, >40% of all adults aged ≥18 years reported all six assessed mitigation behaviors (Table 2). Across all survey waves, reported prevalences of mitigation behaviors were highest among adults aged ≥60 years and lowest among those aged 18–29 years (Table 1) (Supplementary Figure 1: https://stacks.cdc.gov/view/cdc/95944). Age was also significantly associated with the cumulative number of reported mitigation behaviors across all survey waves, with young adults reporting engaging in fewer mitigation behaviors compared with older adults overall and at all time points (Table 2) (Figure).
Among adults who reported face mask use at each time point, a significantly higher percentage reported other mitigation behaviors compared with those who did not report mask use (Supplementary Figure 2: https://stacks.cdc.gov/view/cdc/95945). Among adults who did not report mask use, all other reported mitigation behaviors declined significantly from the April 20–26 wave to early June. Other mitigation behaviors also decreased over time among those who reported mask use, but to a much lesser extent, and only significantly for washing hands, maintaining a 6-foot distance, and cancelling or postponing social events. A higher percentage of adults who reported mask use also reported a higher cumulative number of other mitigation behaviors during the same period, compared with adults who did not report mask use (Figure). By early June, >45% of adults who did not report mask use reported one or fewer other mitigation behaviors (Figure). Overall, a significant positive association between age and the cumulative number of reported mitigation behaviors persisted over time among those who did and those who did not report mask use (Figure).
Discussion
This report provides four important insights into the practice of mitigation behaviors among U.S. adults to prevent the spread of SARS-CoV-2. First, the majority of U.S. adults reported engaging in most or all of the six mitigation behaviors assessed. Second, age was an important determinant of engagement in mitigation behaviors overall. A smaller percentage of adults aged <60 years, particularly those aged 18–29 years, reported engaging in the mitigation behaviors assessed compared with adults aged ≥60 years. Third, while reported use of face masks increased significantly across all age groups over time, other reported mitigation behaviors declined or did not change significantly across age groups. Finally, compared with adults who reported wearing a mask, those who did not report mask use also reported engaging in significantly fewer other mitigation behaviors during the same period, with significant declines in all other behaviors from April to June.
CDC recommends multiple, concurrent mitigation behaviors to most effectively reduce the spread of COVID-19 (6). Fewer reported mitigation behaviors among young adults might contribute to the high incidence of confirmed COVID-19 cases in this age group (4). Older adults might be more concerned about COVID-19, based on their higher risk for severe illness compared with that of younger adults (7). Young adults might also be less likely to engage in mitigation behaviors because of social, developmental, and practical factors (8,9). Across age groups, increases in mask use and decreases in other mitigation behaviors might reflect elevated promotion of mask use over time, along with the lifting of shelter-in-place orders and reopening of business, service, hospitality and other sectors.
Significant declines in self-reported mitigation behaviors among those not reporting mask use suggests that a minority of persons might be increasingly resistant to COVID-19 mitigation behaviors or unable to engage in mitigation behaviors because of the constraints introduced by their return to work, school, or other settings. Effectively promoting engagement in mitigation behaviors among young adults will require moving beyond education to addressing barriers to mitigation behaviors as the pandemic and the response evolve. Strategies might include engaging trusted leaders and social media influencers to improve social acceptability of mitigation behaviors, offering practical tips for engagement, and appealing to personal values. Strategies also might include addressing social and emotional challenges potentially associated with social distancing behaviors, and engaging communities, businesses, employers and institutes of higher education to ensure mitigation behaviors are both feasible and actively encouraged where young adults work, study, and engage in recreational activities. Similar targeted strategies can be used to promote use of recommended mitigation behaviors among all adults.
The findings in this report are subject to at least three limitations. First, survey questions did not ask about consistency, adequacy, or frequency of mitigation behaviors in alignment with public health recommendations and thus might overestimate the real prevalence of mitigation behaviors. For example, the survey item “wore a face mask” did not ask whether a mask was worn over the nose and mouth in public settings and when around persons who are ill or those who live outside of one’s household. Similarly, the survey item “washed or sanitized hands” did not specify frequency of handwashing or handwashing in situations associated with higher risk of exposure to SARS-CoV-2 (e.g., while in a public place) nor did it specify that hands were washed often with soap and water for at least 20 seconds or that sanitizer containing at least 60% alcohol was used. Second, the survey item “avoided some or all restaurants” did not specify type of restaurant service (e.g., curbside pick-up versus dining in), which might underestimate risk mitigation, as on-site dining has been associated with an increased risk for acquiring COVID-19 (10). Finally, all results depend on self-report and thus social desirability and recall bias might result in over- or underestimation of reported mitigation behaviors.
These findings suggest that lower engagement in social mitigation behaviors among younger adults might be one possible reason for the increased incidence of confirmed COVID-19 cases in this group, which began in June 2020 and preceded increases among persons aged ≥60 years by 4–15 days (4). Better understanding of barriers and motivators associated with participation in mitigation behaviors is needed to effectively employ strategies that promote engagement of younger adults and others who are not currently engaging in mitigation behaviors. Reaching these groups through targeted channels, trusted leaders, and influencers at national, state, and local levels has the potential to improve use and effectiveness of critical public health strategies to protect persons of all ages by preventing the spread of SARS-CoV-2.
Corresponding author: Helena Hutchins, [email protected].
1CDC COVID-19 Response Team; 2Data Foundation, Washington, DC; 3Division of Human Development and Disability, National Center on Birth Defects and Developmental Disabilities, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Joseph Willey reports grants from the David and Louise Packard Foundation and the Alfred P. Sloan Foundation (both partial funders of the COVID Impact Survey) during the conduct of the study. No other potential conflicts of interest were disclosed.
* The number of interviews conducted was 2,190 in April, 2,238 in May, and 2,047 in June 2020.
† https://www.census.gov/programs-surveys/cps.html
§ The COVID-19 Impact Survey is conducted by NORC at the University of Chicago. The NORC Institutional Review Board (FWA00000142) reviewed and approved the study protocol to protect the rights and welfare of human subjects.
¶ Respondents could select all behaviors that applied. All 19 possible responses included 1) canceled a doctor appointment; 2) wore a face mask; 3) visited a doctor or hospital; 4) canceled or postponed work activities; 5) canceled or postponed school activities; 6) canceled or postponed dentist or other appointment; 7) canceled outside housekeepers or caregivers; 8) avoided some or all restaurants; 9) worked from home; 10) studied at home; 11) canceled or postponed pleasure, social, or recreational activities; 12) stockpiled food or water; 13) avoided public or crowded places; 14) prayed; 15) avoided contact with high-risk persons; 16) washed or sanitized hands; 17) kept six feet distance from those outside my household; 18) stayed home because I felt unwell; and 19) wiped packages entering my home.
** https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html.
†† https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/personal-social-activities.html.
§§ https://www.whitehouse.gov/wp-content/uploads/2020/03/03.16.20_coronavirus-guidance_8.5x11_315PM.pdf.
References
- CDC. Coronavirus disease 2019 (COVID-19): how to protect yourself and others. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- Fisher KA, Barile JP, Guerin RJ, et al. Factors associated with cloth face covering use among adults during the COVID-19 pandemic—United States, April and May 2020. MMWR Morb Mortal Wkly Rep 2020;69:933–7. CrossRef PubMed
- Wozniak A, Willey J, Benz J, Hart N. COVID Impact Survey: Version 2 [dataset]. Chicago, IL: National Opinion Research Center, 2020. https://www.covid-impact.org/
- Boehmer TK, DeVies J, Caruso E, et al. Changing age distribution of the COVID-19 pandemic—United States, May–August 2020. MMWR Morb Mortal Wkly Rep 2020;69:1404–9. CrossRef PubMed
- Battaglia M, Izrael D, Hoaglin D, Frankel M. Practical considerations in raking survey data. Surv Pract 2009;2:1–10. CrossRef
- CDC. Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/community/community-mitigation.html
- Schaeffer K, Rainie L. Experiences with the COVID-19 outbreak can vary for Americans of different ages. Washington, DC: Pew Research Center; 2020. https://www.pewresearch.org/fact-tank/2020/06/16/experiences-with-the-covid-19-outbreak-can-vary-for-americans-of-different-ages/
- The Harris Poll. COVID-19 Survey Wave 16, June 13–16, 2020. Rochester, NY: The Harris Poll; 2020. https://theharrispoll.com/wp-content/uploads/2020/06/Wave-16_banner-1_no-BP.pdf
- Johnson SB, Blum RW, Giedd JN. Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy. J Adolesc Health 2009;45:216–21. CrossRef PubMed
- Fisher KA, Tenforde MW, Feldstein LR, et al. ; IVY Network Investigators; CDC COVID-19 Response Team. Community and close contact exposures associated with COVID-19 among symptomatic adults ≥18 years in 11 outpatient health care facilities—United States, July 2020. MMWR Morb Mortal Wkly Rep 2020;69:1258–64. CrossRef PubMed
Abbreviations: CI = confidence interval; COVID-19 = coronavirus disease 2019.
* Wore a face mask, washed or sanitized hands, kept 6 feet of distance, avoided public or crowded places, canceled or postponed pleasure, social, or recreational activities and avoided some or all restaurants.
† Chi-square p-value <0.05 for differences across age groups, by survey wave.
§ Test for trend for overall change over time: p-value <0.001.
¶ Test for trend for overall change over time for “avoided public or crowded places”: p-value = 0.002.
Abbreviations: CI = confidence interval; COVID-19 = coronavirus disease 2019.
* Wore a face mask, washed or sanitized hands, kept 6 feet of distance, avoided public or crowded places, canceled or postponed pleasure, social, or recreational activities and avoided some or all restaurants.
† Test for trend for overall change in behavior over time p-value <0.001.
§ Chi-square p-value <0.01 for differences across age groups, by survey wave.
¶ Chi-squared p–value <0.05 for differences across age groups, by survey wave.
 FIGURE. Percentage distribution of cumulative number of reported mitigation behaviors,* by age group and reported face mask use — COVID Impact Survey, United States, April–June 2020†,§,¶,**,††,§§
FIGURE. Percentage distribution of cumulative number of reported mitigation behaviors,* by age group and reported face mask use — COVID Impact Survey, United States, April–June 2020†,§,¶,**,††,§§
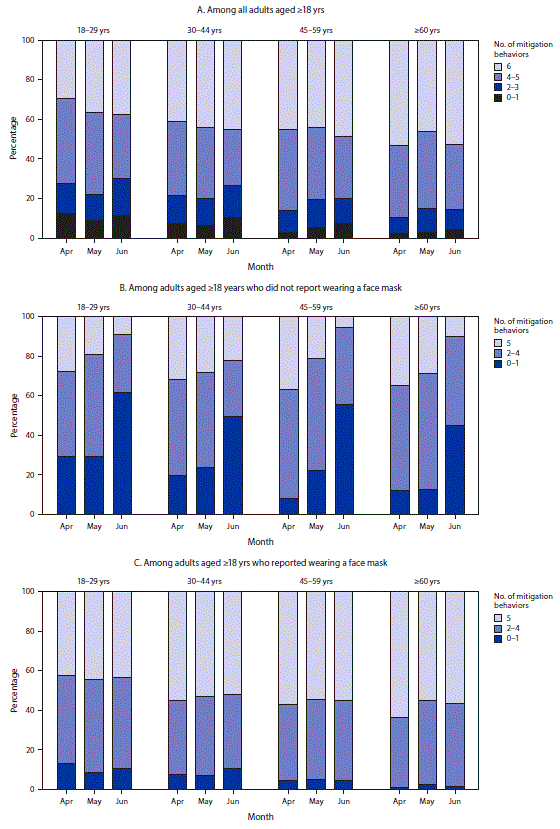
Abbreviation: COVID-19 = coronavirus disease 2019.
* Wore a face mask; washed or sanitized hands; kept 6 feet of distance; avoided public or crowded places; canceled or postponed pleasure, social, or recreational activities; and avoided some or all restaurants.
† Weighted to be representative of noninstitutionalized U.S. adults; values <5% not shown.
§ Trend for overall change in behavior over time, p-value <0.001.
¶ Chi-squared p-value <0.001 for differences in cumulative number of mitigation behaviors reported across age groups, within all survey waves.
** Chi-squared p-value <0.05 for differences in cumulative number of mitigation behaviors reported across age groups, within April and June waves only.
†† Not inclusive of the survey item “wore a face mask.”
§§ Trend for overall change in behavior over time p-value <0.05 (among those who reported wearing a mask: p-value = 0.003).
Suggested citation for this article: Hutchins HJ, Wolff B, Leeb R, et al. COVID-19 Mitigation Behaviors by Age Group — United States, April–June 2020. MMWR Morb Mortal Wkly Rep 2020;69:1584–1590. DOI: http://dx.doi.org/10.15585/mmwr.mm6943e4.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to [email protected].