mitochondrial disease
Our editors will review what you’ve submitted and determine whether to revise the article.
- Also called:
- mitochondrial disorder
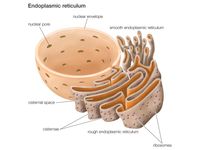
mitochondrial disease, any of several hundred hereditary conditions that result from a functional failure of the mitochondrion, a type of cellular organelle. Mitochondrial diseases can emerge at any age and are enormously diverse in their clinical and molecular features. They range in severity from relatively mild disease that affects just a single organ to debilitating and sometimes fatal illness that affects multiple organs. The wide spectrum of symptoms poses significant challenges to the diagnosis of conditions associated with mitochondrial dysfunction. At least 1 in every 5,000 persons worldwide is affected by mitochondrial disease.
Although some mitochondrial diseases are caused by mutations in the mitochondrial genome (mtDNA), the majority of the conditions are the result of mutations in genes in the nuclear genome, which encodes a number of proteins that are exported and transported to mitochondria in the cell. The proteins are assembled in mitochondria to form the electron transport chain (ETC), the primary energy-generating apparatus of cells. The transfer of electrons from one protein component to the next ultimately enables cells to produce energy in the form of adenosine triphosphate (ATP), which is the main form of energy used by cells and organs in the body. Deficiency in any of the proteins that make up the ETC can impair ATP production and lead to the buildup of unused intermediates (the initial sugar and fat molecules that enter the ETC) and reactive oxygen species (ROS; a free radical containing oxygen). Unused intermediates may react with other molecules, resulting in the generation of damaging by-products such as lactic acid, while ROS may react with various cellular molecules, causing oxidative stress and cell death.

Signs and symptoms of mitochondrial disease vary, depending on the organ or organ systems involved. Possible indications include developmental delay, reduced growth, fatigue, migraine, muscle weakness, muscle pain, cardiomyopathy, liver failure, blindness, optic atrophy (degeneration of the optic nerve), hearing loss, diabetes, and seizures. Clusters of signs and symptoms often emerge, indicating a discrete syndrome. For example, in individuals of age three months to two years, failure to thrive, progressive neurological degeneration (with decreased muscle tone, uncoordinated movement, and involuntary and repetitive muscle contraction), and visual, respiratory, and cardiac problems are characteristic of Leigh syndrome. Kearns-Sayre syndrome, on the other hand, is characterized primarily by progressive weakness or paralysis of the eye muscles and retinopathy (damage to the light-sensing retina of the eye), which can result in drooping eyelids and a loss of vision; onset typically is before age 20.
The diagnosis of mitochondrial disease is based on clinical features and, when possible, the results of genetic testing. Maternal family history of disease may provide important diagnostic insight, since inherited mitochondrial diseases are passed from the mother to her offspring and are transmitted strictly down maternal family lines. Persons affected by mitochondrial diseases may receive genetic counseling to assess the risk of passing on an inherited disorder.
Treatment for mitochondrial diseases is supportive. Optical aids, including lens replacement, and hearing aids, such as cochlear implants, may benefit individuals with visual or auditory deficits. Some patients may benefit from implanted cardiac pacemakers or defibrillators. Supportive therapies for deficiencies in specific ETC components may include oral administration of substances such as coenzyme Q10, l-creatine (creatine monohydrate), or riboflavin. Exercise may also help relieve symptoms in some individuals.