 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
| ||||||||||
|
|
|
|
|
Persons using assistive technology might not be able to fully access information in this file. For assistance, please send e-mail to: [email protected]. Type 508 Accommodation and the title of the report in the subject line of e-mail. CDC's 60th Anniversary: Director's Perspective --- James O. Mason, M.D., Dr.P.H., 1983--1989An erratum has been published for this article. To view the erratum, please click here. New Responsibilities Bring New ChallengesThe growing momentum toward expanding CDC's responsibilities beyond infectious diseases gained strength during the 1980s. Tremendous advances in controlling infectious diseases had dramatically reduced illness and death from many long-standing health threats. In addition, the detrimental effects of chronic and other noncommunicable diseases on the nation's health were rapidly increasing. Programs to address cancer, heart disease, diabetes, and other leading killers became central to CDC's focus. Yet, for much of this decade, a newly emerging infectious disease would demand the skills and talents of persons across the agency. These new responsibilities led to additional funding, programs, staff, and partnerships for the growing agency, while introducing a host of new challenges. Preventing Chronic DiseasesAmong the most targeted causes of chronic diseases was smoking. Steps to reduce the harmful effects of tobacco products had steadily increased throughout the U.S. Department of Health and Human Services (DHHS). CDC was heavily involved in these activities and faced pressures from industry and political fronts. In October 1984, Congress enacted the first major legislation on smoking and health in 15 years, the Comprehensive Smoking Education Act, Public Law 98-474. This legislation required stronger and more specific health warnings on all cigarette packages and advertisements and outlined specific responsibilities for DHHS. Among these were directives to expand activities on smoking and health and to issue a biennial report to Congress. In 1986, the DHHS Office on Smoking and Health was transferred to CDC and joined with CDC's programs to produce the first of these reports, Smoking and Health: A National Status Report (1), providing a comprehensive look at this important public health problem across national, state, and local levels. In his cover letter distributing the report to Congress, the Secretary of Health and Human Services urged all jurisdictions to adopt a minimum age of 18 years for persons to legally purchase tobacco products, stating that "Enactment and enforcement of such legislation could have a strong preventive effect on early uptake of cigarettes and other tobacco products." Included in the report were findings that 12 states had no age-related tobacco restrictions, and 14 of those with such laws had set the minimum age for purchasing tobacco products at younger than 18 years. The agency's expanding smoking-related programs advanced plans to create a chronic disease center at CDC, and in 1988, the Center for Chronic Disease Prevention and Health Promotion became a reality. Focus on Injury and ViolenceCDC's programs to prevent injury and violence also were gaining prominence. As had been shown with chronic diseases, many of the same tools that had long proven effective in preventing and reducing infectious diseases (e.g., surveillance, epidemiologic research, education, and communication) could be used to address both unintentional and intentional injuries. In 1985, the Institute of Medicine published a report, Injury in America: A Continuing Public Health Problem (2), drawing attention to and recommending steps to stem this rising public health problem; among these steps was the establishment of a center for injury control at CDC. Broadening their expertise, CDC's violence program within the Center for Health Promotion and Education joined with CDC's injury program in 1986 to become the Division of Injury Prevention and Control in the Center for Environmental Health. Through this division, CDC undertook additional steps to address these alarming threats (e.g., homicide, suicide, and motor-vehicle traffic deaths), including funding of injury control research centers at universities throughout the country to conduct research in prevention, acute care, and rehabilitation. These measures paved the way for establishment of the National Center for Injury Prevention and Control at CDC in 1992. Agent Orange StudiesAs Bill Foege described in his Director's Perspective (3), CDC's expanding work toward reducing noninfectious health conditions brought with it many new challenges. Under legislation enacted in 1979 and 1981, Congress directed the Veterans Administration (VA) to conduct investigations into the health of U.S. Vietnam veterans in response to growing concerns from veterans that exposure to the defoliant mixture "Agent Orange," used widely in Vietnam, had affected their health and that of their children. In January 1983, CDC was assigned responsibility through an interagency agreement with the VA for designing, conducting, and analyzing data from these studies. Under authorization from Congress, CDC began three epidemiologic studies: the Agent Orange Exposure Study designed to evaluate the long-term health effects of exposure to herbicides, particularly Agent Orange, among Vietnam veterans; 2) the Vietnam Experience Study, a comprehensive study examining the occurrence of adverse health effects among Vietnam veterans; and 3) the Selected Cancers Study to determine whether Vietnam veterans were at increased risk for certain types of cancers possibly related to exposure to dioxin, a contaminant found in Agent Orange. The Agent Orange Exposure Study was abandoned as unfeasible in 1987. Validation testing in a sample of veterans who served in Vietnam at the time and location of heaviest Agent Orange spraying found that none of the indirect methods for assessing exposure showed any meaningful association with current levels of dioxin in blood. Moreover, no method could be identified for using military records or self-reported exposure to distinguish between U.S. Army ground combat troops who were and were not exposed to Agent Orange in Vietnam. The Vietnam Experience Study went beyond herbicide exposure to examine many factors that could have adversely affected Vietnam veterans, including the psychological stresses of war, possible exposure to various infectious diseases, reproductive outcomes, and possible misuse of drugs and alcohol. The study involved more than 7,000 men who had served in Vietnam during 1965--1971 and a similar number of veterans who had served elsewhere during the same period. The study found that the Vietnam veterans more frequently reported health problems for themselves and their children, compared with the non-Vietnam veterans, but very few differences between the two groups were found on medical and laboratory examinations, including hospital birth records. However, problems such as depression, anxiety, and combat-related post-traumatic stress disorder were found to be more common among the Vietnam veterans (4). The Selected Cancers Study assessed the risk for non-Hodgkin's lymphoma, soft tissue sarcoma, Hodgkin's disease, nasopharyngeal cancer, and primary liver cancer among Vietnam veterans. Compared with men who did not serve in Vietnam, Vietnam veterans had an increased risk for non-Hodgkin's lymphoma but not for the other four cancers. Among those with non-Hodgkin's lymphoma, however, little difference could be found with respect to their reporting of experiences that might have been associated with increased risk for exposure to Agent Orange. Although CDC remained focused on reporting the evidence and the limitations in its interpretation, controversy surrounded these studies and their findings. Emergence of AIDS Brings Unprecedented Public Health ConflictThe formidable challenges presented by CDC's broadening responsibilities underscored the importance of strictly adhering to science in presenting findings and developing policy. This lesson would prove even more critical as a new infectious disease began emerging in young, homosexual men in the United States, challenging the public health community in unforeseen ways and eventually changing world health. Fully entrenched by the time it was recognized in 1981, the disease, eventually given the name acquired immunodeficiency syndrome (AIDS), reintroduced the public to fear of infectious diseases and divided the country across social, religious, and political lines. Before AIDS, public fear of infectious diseases had largely subsided because of the availability and widespread use of vaccines and antibiotics. Many believed most infectious diseases were curable and no longer life-threatening, affording a new level of health not enjoyed by previous generations. AIDS abruptly corrected this misperception (Figure 1), emerging as a new health threat with devastating consequences and a host of medical, ethical, legal, and economic implications. Developing Evidence-Based GuidelinesNot only was the new condition baffling, the myriad associated diseases, termed "opportunistic infections" because they were usually only seen in persons with drug-suppressed or otherwise severely compromised immune systems, were unfamiliar to most physicians and scientists. However, within 1 year of the first case reports, a case definition had been developed and all major routes of transmission had been identified. In March 1983, CDC published the first set of guidelines for preventing the disease (5). Based on the best available science at the time, these recommendations proved essentially correct and have not been revised significantly. In 1984, the cause of the disease was determined to be a previously unrecognized retrovirus, first termed human T-lymphotropic virus type III/lymphadenopathy-associated virus (HTLV-III/LAV) and later renamed human immunodeficiency virus (HIV). In March 1985, a test to detect antibodies to the virus was licensed by the Food and Drug Administration (FDA) for use in screening donated blood and plasma. Although the test was not approved for individual testing, public health officials recognized that many at-risk persons would seek testing at blood banks to learn their infection status. By this time, sufficient funds had been authorized by Congress to enable CDC to begin funding AIDS prevention activities in state and local health departments. Through cooperative agreements, CDC awarded funds to 55 state and local health departments to establish alternate testing sites for at-risk persons to obtain antibody tests free of charge outside the blood-bank setting. Such sites were established both to decrease potential false-negative donations and to ensure that persons wishing to be tested would receive appropriate pre- and post-test counseling and referrals. Use of the antibody test for individual testing was approved by FDA in 1986. The ability to test persons for the virus offered new opportunities for prevention and for treatment to possibly delay the onset of the disease. Unfortunately, this medical advancement also unleashed a new set of fears among an already stigmatized population, especially regarding increased discriminatory actions related to education, employment, health care, and insurance. Scientifically, these early years of AIDS were characterized by unprecedented progress toward understanding a new, highly complex infectious disease. In 1985, the first AIDS conference was held, and the World Health Organization formed a network of AIDS collaborating centers. By the end of 1986, CDC had published nearly 100 MMWR reports related to AIDS. These reports included recommendations to prevent transmission of the virus through transfusions, transplants, patient care, and perinatal exposure; workplace and school-based guidelines; and critical reports from state and local health departments outlining the epidemic's impact in their areas. CDC's AIDS surveillance programs were among the most comprehensive disease-tracking measures ever undertaken. These programs yielded data that highlighted growing epidemics outside of major metropolitan areas and among minority populations, allowing for more targeted prevention measures and funding. Fear Affects Public PolicyDespite solid scientific advances, no epidemic in history has engendered a greater level of controversy. Divisive views over the epidemic's earliest and most severely affected populations, homosexual/bisexual men and intravenous drug users, undoubtedly hindered progress on many fronts, including risk communication and funding for prevention and research. Some in Congress claimed that AIDS spending was exorbitant, disproportional to the magnitude of the problem, while others argued that inadequate funding was slowing research on testing, treatment, and vaccine development. The public also became involved in these disputes, disagreeing on transmission risks, populations that should be tested, and restrictions on infected persons. The media fueled their interests. In describing results from a 1985 poll of more than 2,000 persons, the New York Times reported that "51 percent of the respondents supported a quarantine of acquired immune deficiency syndrome patients, 48 percent would approve identity cards for those who have taken tests indicating the presence of AIDS antibodies, and 15 percent supported tattooing those with AIDS" (6). Although these arguments were vocalized as focusing on rights of the public versus rights of AIDS patients, in reality they were driven by fear. The medical and scientific community had difficulty communicating the risks associated with this new disease with the same level of certainty demanded by the public. Studies conducted among family members of AIDS patients had provided strong evidence of the lack of transmission from casual contact. However, many persons, including lawmakers, believed otherwise and were not readily dissuaded. In particular, school attendance by children with AIDS was the subject of intense debate. CDC's 1985 recommendations on education and foster care for children with HIV/AIDS stated that decisions regarding the type of education and care setting for infected children should be made on an individual basis but that "For most infected school-aged children, the benefits of an unrestricted setting would outweigh the risks of their acquiring potentially harmful infections in the setting and the apparent nonexistent risk of transmission of HTLV-III/LAV" (7). Soon after the release of these guidelines in late August 1985, the Washington Post ran an op-ed piece entitled, "Worry about the Survival of Society First; Then AIDS Victims' Rights," which was picked up by newspapers across the country (8,9). Playing to the public's fear and skepticism, the editorial argued that many of the laws that had been enacted to protect AIDS patients from discrimination were misguided and cited CDC's recent guidelines as remiss. In many areas of the country, these recommendations were met with staunch opposition. In Florida, the parents of three HIV-infected hemophilic sons, Ricky, Robert, and Randy Ray, were plaintiffs in a federal lawsuit against their local school board to allow their children to attend public school. A week after the court's ruling in favor of the Rays, their home was burned down. In Indiana, the experiences endured by a young man named Ryan White would ultimately change public opinion on AIDS throughout the world and lead to specifically designated federal resources for AIDS patients through the 1990 Ryan White Comprehensive AIDS Resources Emergency (CARE) Act. At CDC, measures to expand surveillance and case reporting and to develop new prevention guidelines required dedicated consensus building that went beyond the medical and scientific community to include affected persons, special interest and political groups, and the public. Throughout these processes, CDC worked to ensure that these new recommendations and guidelines reflected the best available science, a commitment that has served public health well. For example, CDC's 1988 recommendations for preventing HIV transmission in health-care settings (10) recommended that blood and certain body fluids from every single patient be viewed as potentially infectious for HIV or other bloodborne pathogens. These guidelines became known as "universal blood and body fluid precautions" or "universal precautions" and led to permanent changes in health-care practices throughout the world. Strengthening State and Local Public Health InfrastructuresBy the mid-1980s, both funding and political support were available to launch widespread public information campaigns, viewed as critical in stemming the epidemic and enabling those already infected to receive treatment and other services. CDC's National AIDS Hotline was started in 1983 to enhance surveillance for the disease, but its role quickly expanded to address the urgent need for disseminating accurate and timely information. In 1987, CDC established the National AIDS Clearinghouse to distribute printed materials on AIDS. The same year, CDC launched America Responds to AIDS, a substantial, nationwide public information campaign that had been developed through extensive formative research (11). Over the next 4 years, five separate phases of informational materials were developed and released to the general public, ranging from basic information on the disease to specific information for different risk groups. The largest of these came in 1988, when more than 107 million copies of the brochure Understanding AIDS were delivered to homes and residential post office boxes in the United States (Figure 2). A Spanish-language version also was distributed in Puerto Rico and other predominantly Spanish-speaking areas. The brochure, developed by CDC in consultation with Surgeon General C. Everett Koop, other health experts, and public citizens, marked the first time the federal government had attempted to contact every resident directly by mail regarding a public health problem (12). Koop's open stance against smoking had made him a well-recognized public health official, and his commitment to educating the public on HIV/AIDS made him a highly effective and credible spokesperson in this effort. In addition to expanded funding for AIDS surveillance and prevention activities at state and local health departments, CDC began funding national and regional minority organizations, community-based organizations, and the faith-based community for these activities in 1988--1989. This increased funding for extramural activities is reflected in CDC's budget for those years, which nearly tripled from fiscal years 1983--1989 (Figure 3) without a commensurate increase in full-time employees (Figure 4). The systems and services developed and implemented in response to the AIDS epidemic helped build and maintain public health infrastructures at multiple levels and would improve capabilities and serve as a model for other disease detection and prevention measures. During 1981--1989, more than 100,000 cases of AIDS in the United States were reported to CDC, approximately one third of them in 1989 alone (13). Although cases were reported from all 50 states, the District of Columbia, and four U.S. territories, two thirds of the cases were reported from five states: New York, New Jersey, Florida, Texas, and California. In addition, although the epidemic had spread beyond the earliest risk groups of homosexual/bisexual men and intravenous drug users, these groups continued to account for nearly 90% of cases. Today, the epidemic's global impact is staggering, with nearly 40 million persons living with HIV throughout the world (14). The fear of the disease that so adversely affected the U.S. response during the early years of the epidemic has largely subsided in this country, dissolving much of the resistance to new policies and procedures and enabling better acceptance and delivery of new prevention and treatment strategies. A clear example of this change is reflected in CDC's new HIV-testing recommendations (15). Published in September 2006, these evidence-based recommendations call for nearly universal testing of patients in health-care settings, a strategy that would not have been possible to put forward as recently as a decade ago. In many of the world's most heavily affected regions, however, fear and lack of education about the disease continue to impede prevention measures and stigmatize infected persons. As new funding and partners are united globally to address the pandemic, primary prevention measures must first focus on ending the fear. An Expanded AgencyChange, expansion, and growing domestic and international visibility characterized CDC's fourth decade. Exacting science and honest risk communication proved to be the agency's most effective prevention tools. Lessons learned from past successes and challenges will serve CDC well as its roles and responsibilities toward protecting the nation's health continue to expand. References
  Figure 1  Return to top. Figure 2  Return to top. Figure 3 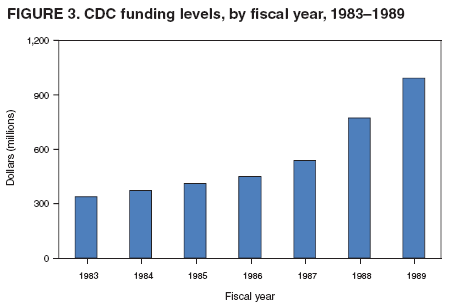 Return to top. Figure 4  Return to top.
All MMWR HTML versions of articles are electronic conversions from ASCII text into HTML. This conversion may have resulted in character translation or format errors in the HTML version. Users should not rely on this HTML document, but are referred to the electronic PDF version and/or the original MMWR paper copy for the official text, figures, and tables. An original paper copy of this issue can be obtained from the Superintendent of Documents, U.S. Government Printing Office (GPO), Washington, DC 20402-9371; telephone: (202) 512-1800. Contact GPO for current prices. **Questions or messages regarding errors in formatting should be addressed to [email protected].Date last reviewed: 12/20/2006 |
|||||||||
|