Characteristics of Persons Who Died with COVID-19 — United States, February 12–May 18, 2020
Weekly / July 17, 2020 / 69(28);923-929
On July 10, 2020, this report was posted online as an MMWR Early Release.
Please note: This report has been corrected.
Jonathan M. Wortham, MD1; James T. Lee, MD1; Sandy Althomsons, MHS1; Julia Latash, MPH2; Alexander Davidson, MPH2; Kevin Guerra, MPH2; Kenya Murray, MPH2; Emily McGibbon, MPH2; Carolina Pichardo2; Brian Toro2; Lan Li, MPH2; Marc Paladini, MPH2; Meredith L. Eddy, MPH2; Kathleen H. Reilly, PhD2; Lisa McHugh, PhD3; Deepam Thomas, MPH3; Stella Tsai, PhD3; Mojisola Ojo, MPH3; Samantha Rolland, PhD4; Maya Bhat, MPH4; Katherine Hutchinson, PhD4; Jennifer Sabel, PhD4; Seth Eckel, MPH5; Jim Collins, MPH5; Catherine Donovan, PhD6; Anna Cope, PhD6; Breanna Kawasaki, MPH7; Sarah McLafferty, MPH7; Nisha Alden, MPH7; Rachel Herlihy, MD7; Bree Barbeau, MPH8; Angela C. Dunn, MD8; Charles Clark, MPH9; Pamela Pontones, MPH9; Meagan L. McLafferty, MPH10; Dean E. Sidelinger, MD10; Anna Krueger, MS11; Leslie Kollmann12; Linnea Larson, MPH12; Stacy Holzbauer, DVM1,12; Ruth Lynfield, MD12; Ryan Westergaard, MD13; Richard Crawford, MD13; Lin Zhao, MD13; Jonathan M. Bressler, MPH14; Jennifer S. Read, MD15,16; John Dunn, DVM17; Adele Lewis, MD17; Gillian Richardson, MPH18; Julie Hand, MSPH18; Theresa Sokol, MPH18; Susan H. Adkins, MD1; Brooke Leitgeb, MS1; Talia Pindyck, MD1; Taniece Eure, MPH1; Karen Wong, MD1; Deblina Datta, MD1; Grace D. Appiah, MD1; Jessica Brown, PhD1; Rita Traxler, MHS1; Emilia H. Koumans, MD1; Sarah Reagan-Steiner, MD1 (View author affiliations)
View suggested citationSummary
What is already known about this topic?
COVID-19 mortality is higher in persons with underlying medical conditions and in those aged ≥85 years.
What is added by this report?
Analysis of supplementary data for 10,647 decedents in 16 public health jurisdictions found that a majority were aged ≥65 years and most had underlying medical conditions. Overall, 34.9% of Hispanic and 29.5% of nonwhite decedents were aged <65 years, compared with 13.2% of white, non-Hispanic decedents. Among decedents aged <65 years, a total of 7.8% died in an emergency department or at home.
What are the implications for public health practice?
Understanding factors contributing to racial/ethnic mortality differences and out-of-hospital deaths might inform targeted communication to encourage persons in at-risk groups to practice preventive measures and promptly seek medical care if they become ill.
During January 1, 2020–May 18, 2020, approximately 1.3 million cases of coronavirus disease 2019 (COVID-19) and 83,000 COVID-19–associated deaths were reported in the United States (1). Understanding the demographic and clinical characteristics of decedents could inform medical and public health interventions focused on preventing COVID-19–associated mortality. This report describes decedents with laboratory-confirmed infection with SARS-CoV-2, the virus that causes COVID-19, using data from 1) the standardized CDC case-report form (case-based surveillance) (https://www.cdc.gov/coronavirus/2019-ncov/php/reporting-pui.html) and 2) supplementary data (supplemental surveillance), such as underlying medical conditions and location of death, obtained through collaboration between CDC and 16 public health jurisdictions (15 states and New York City).
Case-based surveillance
Demographic and clinical data about COVID-19 cases are reported to CDC from 50 states, the District of Columbia, New York City, and U.S. territories using a standardized case-report form (case-based surveillance) or in aggregate. Data on 52,166 deaths from 47 jurisdictions among persons with laboratory-confirmed COVID-19 were reported individually to CDC via case-based surveillance during February 12–May 18, 2020. Among the 52,166 decedents, 55.4% were male, 79.6% were aged ≥65 years, 13.8% were Hispanic/Latino (Hispanic), 21.0% were black, 40.3% were white, 3.9% were Asian, 0.3% were American Indian/Alaska Native (AI/AN), 0.1% were Native Hawaiian or other Pacific Islander (NHPI), 2.6% were multiracial or other race, and race/ethnicity was unknown for 18.0%. (Table 1). Median decedent age was 78 years (interquartile range (IQR) = 67–87 years). Because information about underlying medical conditions was missing for the majority of these decedents (30,725; 58.9%), data regarding medical conditions were not analyzed further using the case-based surveillance data set. Because most decedents reported to the supplementary data program were also reported to case-based surveillance, no statistical comparisons of the decedent characteristics between the data sets were made.
Supplemental surveillance
To collect more complete data on race/ethnicity, selected underlying medical conditions* by age, and clinical course, CDC solicited supplementary information from medical charts and death certificates of decedents with laboratory-confirmed COVID-19 from state, territorial, and local public health departments. The supplementary data request also sought information on locations of death, which is not collected routinely on the CDC case-report form. Among 56 public health departments contacted by CDC, 16† provided supplementary data on 10,647 COVID-19 deaths that occurred during February 12–April 24, 2020.
Among the 10,647 COVID-19 decedents for whom supplementary data were collected, 60.6% were male, 74.8% were aged ≥65 years, 24.4% were Hispanic, 24.9% were black, 35.0% were white, 6.3% were Asian, 0.1% were AI/AN, 0.1% were NHPI, 2.9% were multiracial or other race, and race/ethnicity was unknown for 6.3% (Table 1). Decedent age varied by race and ethnicity; median age was 71 years (IQR = 59–81 years) among Hispanic decedents, 72 years (IQR = 62–81 years) among all nonwhite, non-Hispanic decedents, and 81 years (IQR = 71–88 years) among white decedents. The percentages of Hispanic (34.9%) and nonwhite (29.5%) decedents who were aged <65 years were more than twice those of white decedents (13.2%) (Figure).
At least one underlying medical condition was reported for 8,134 (76.4%) of decedents for whom supplementary data were collected, including 83.1% of decedents aged <65 years. Overall, the most common underlying medical conditions were cardiovascular disease (60.9%), diabetes mellitus (39.5%), chronic kidney disease (20.8%), and chronic lung disease (19.2%) (Table 2). Among decedents aged <65 years, 83.1% had one or more underlying medical conditions. Among decedents aged ≥85 years, 69.5% had one or more underlying medical conditions. Diabetes was more common among decedents aged <65 years (49.6%) than among those aged ≥85 years (25.9%).
Among decedents for whom supplementary data were reported, 8,976 (84.3%) were hospitalized. Among 3,021 (28.4%) with dates of illness onset and death reported, the median interval from illness onset to death was 10 days (IQR = 6–15 days); among 7,794 decedents with hospital admission and death dates, the median interval from hospital admission to death was 5 days (IQR = 3–8 days). Among the decedents, 62.0% died in hospitals. By age group, the largest percentage who died in the emergency department (6.8%) or at home (1.0%) was aged <65 years (combined total = 7.8%), and decreased with increasing age group, whereas the percentage who died in long-term care facilities increased with increasing age and was highest among decedents aged ≥85 years (12.6%).
Among the decedents during February 12–April 24, 2020, for whom supplementary information was provided, 9,997 (93.9%) resided in New York City, New Jersey, or the state of Washington, three areas with early widespread circulation of SARS-CoV-2; the median age among decedents in these three jurisdictions was 75 years, (IQR = 64–84 years). The median age among decedents residing in the other 13 jurisdictions was similar (78 years, [IQR = 68–85 years]).
Discussion
Using national case-based surveillance and supplementary data reported from 16 jurisdictions, characteristics of >10,000 decedents with laboratory-confirmed COVID-19 were described. More than one third of Hispanic decedents (34.9%) and nearly one third (29.5%) of nonwhite decedents were aged <65 years, but only 13.2% of white decedents were aged <65 years. Consistent with reports describing the characteristics of deaths in persons with COVID-19 in the United States and China (2–5), approximately three fourths of decedents had one or more underlying medical conditions reported (76.4%) or were aged ≥65 years (74.8%). Among reported underlying medical conditions, cardiovascular disease and diabetes were the most common. Diabetes prevalence among decedents aged <65 years (49.6%) was substantially higher than that reported in an analysis of hospitalized COVID-19 patients aged <65 years (35%) and persons aged <65 years in the general population (<20%) (5–7). Among decedents aged <65 years, 7.8% died in an emergency department or at home; these out-of-hospital deaths might reflect lack of health care access, delays in seeking care, or diagnostic delays. Health communications campaigns could encourage patients, particularly those with underlying medical conditions, to seek medical care earlier in their illnesses. Additionally, health care providers should be encouraged to consider the possibility of severe disease among younger persons who are Hispanic, nonwhite, or have underlying medical conditions. More prompt diagnoses could facilitate earlier implementation of supportive care to minimize morbidity among individuals and earlier isolation of contagious persons to protect communities from SARS-CoV-2 transmission.
The relatively high percentages of Hispanic and nonwhite decedents aged <65 years were notable. The median age of nonwhite persons (31 years) in the United States is lower than that of white persons (44 years); these differences might help explain the higher proportions of Hispanic and nonwhite decedents among those aged <65 years. The median ages among Hispanic and nonwhite decedents (71 and 72 years, respectively) were 9–10 years lower than that of white decedents (81 years). However, the percentage of Hispanic decedents aged <65 years (33.9%) exceeded the percentage of Hispanic persons aged <65 years in the U.S. population (20%); the percentage of nonwhite COVID-19 decedents aged <65 years (40.2%) also exceeded the overall percentage of nonwhite decedents aged <65 years (23%) in the U.S. population (8). Further study is needed to understand the reasons for these differences. It is possible that rates of SARS-CoV-2 transmission are higher among Hispanic and nonwhite persons aged <65 years than among white persons; one potential contributing factor is higher percentages of Hispanic and nonwhite persons engaged in occupations (e.g., service industry) or essential activities that preclude physical distancing (9). It is also possible that the COVID-19 pandemic disproportionately affected communities of younger, nonwhite persons during the study period (10). Although these data did not permit assessment of interactions between race/ethnicity, underlying medical conditions, and nonbiologic factors, further studies to understand and address these racial/ethnic differences are needed to inform targeted efforts to prevent COVID-19 mortality.
The findings in this report are subject to at least five limitations. First, despite >90% completeness for age and race/ethnicity variables in the supplementary data set, the proportion of missing data for some variables, such as underlying medical conditions, clinical course, and race/ethnicity in case-based surveillance, and location of death, was higher than that for other variables; accordingly, the proportions reported for these variables should be considered minimum proportions rather than robust estimates. Second, reporting practices varied by jurisdiction, and several states bundled underlying medical conditions into organ system–specific categories (e.g., hypertension was included as cardiovascular disease) or did not code specifically for a given condition (e.g., immunosuppression was only specifically coded in 10 of the jurisdictions). These differences in reporting structure precluded evaluations of specific conditions other than diabetes using the entire data set. Third, generalizability of the findings from either data set to all deaths among persons with COVID-19, either within the individual jurisdictions or across the United States, is unknown; COVID-19 testing practices for decedents might differ among jurisdictions. Fourth, information from the supplementary data set provides additional insight into decedent demographic and clinical characteristics; however, these data are a convenience sample from 16 public health jurisdictions. Therefore, because the age-race structure of the underlying population is not known, age-standardized mortality rates could not be calculated. Although more than 90% of decedents resided in just three jurisdictions, and most are represented in case-based surveillance, they represent a subset of deaths reported during this period. Therefore, neither calculations of mortality rates nor statistical comparisons between the demographic characteristics of the decedents with available supplementary data and those from case-based surveillance were possible. Finally, these data were collected during a period before dexamethasone was shown to reduce deaths among ventilated patients; implementation of dexamethasone and other therapeutics, as well as shifts in the ages of patients and geographic locations of cases might affect the generalizability of these data to the current period.
Despite these limitations, this report provides more detailed demographic and clinical information on a subset of approximately 10,000 decedents with laboratory-confirmed COVID-19. Most decedents were aged >65 years and had underlying medical conditions. Compared with white decedents, more Hispanic and nonwhite decedents were aged <65 years. Additional studies are needed to elucidate associations between age, race/ethnicity, SARS-CoV-2 infection, disease severity, underlying medical conditions (especially diabetes), socioeconomic status (e.g., poverty and access to health care), behavioral factors (e.g., ability to comply with mitigation recommendations and maintain essential work responsibilities), and out-of-hospital deaths. Regional and state level efforts to examine the roles of these factors in SARS-CoV-2 transmission and COVID-19-associated deaths could lead to targeted, community-level, mortality prevention initiatives. Examples include health communication campaigns targeted towards Hispanics and nonwhite persons aged <65 years. These campaigns could encourage social distancing and the need for wearing cloth face coverings in public settings. In addition, health care providers should be encouraged to consider the possibility of disease progression, particularly in Hispanic and nonwhite persons aged <65 years and persons of any race/ethnicity, regardless of age, with underlying medical conditions, especially diabetes.
Corresponding author: Jonathan M. Wortham, [email protected].
1CDC COVID-19 Response Team; 2New York City Department of Health and Mental Hygiene; 3New Jersey Department of Health; 4Washington State Department of Health; 5Michigan Department of Health and Human Services; 6North Carolina Department of Health and Human Services; 7Colorado Department of Public Health and Environment; 8Utah Department of Health; 9Indiana State Department of Health; 10Oregon Health Authority; 11Maine Center for Disease Control and Prevention; 12Minnesota Department of Health; 13Wisconsin Department of Health Services; 14Alaska Department of Health and Social Services; 15Vermont Department of Health, 16University of Vermont Medical Center, 17Tennessee Department of Health, 18Louisiana Department of Health.
* Underlying medical conditions include cardiovascular disease (congenital heart disease, coronary artery disease, congestive heart failure, hypertension, cerebrovascular accident/stroke, valvular heart disease, conduction disorders or dysrhythmias, other cardiovascular disease); diabetes mellitus; chronic lung disease (chronic obstructive pulmonary disease/emphysema, asthma, tuberculosis, other chronic lung diseases); immunosuppression (cancer, human immunodeficiency virus (HIV) infection, identified as being immunosuppressed); chronic kidney disease (chronic kidney disease, end-stage renal disease, other kidney diseases); neurologic conditions (dementia, seizure disorder, other neurologic conditions); chronic liver disease (cirrhosis, alcoholic hepatitis, chronic liver disease, end-stage liver disease, hepatitis B, hepatitis C, nonalcoholic steatohepatitis, other chronic liver diseases); obesity (body mass index ≥30 kg/m2). Information was collected from decedent medical records or death certificates. For 10 states (10,461 decedents), information was abstracted into state surveillance data structures and transmitted to CDC. For six states (186 decedents), the medical records and death certificates were sent to CDC and abstracted using a standardized form.
† Alaska Department of Health and Social Services; Colorado Department of Public Health and Environment; Indiana State Department of Health; Louisiana Department of Health; Maine Center for Disease Control and Prevention; Michigan Department of Health and Human Services; Minnesota Department of Health; New Jersey Department of Health; New York City Department of Health and Mental Hygiene; North Carolina Department of Health and Human Services; Oregon Health Authority; Tennessee Department of Health; Utah Department of Health; Vermont Department of Health; Washington State Department of Health; Wisconsin Department of Health Services.
References
- CDC. Coronavirus disease 2019: cases in U.S. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html
- Bialek S, Boundy E, Bowen V, et al.; CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep 2020;69:343–6. CrossRef PubMed
- Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020. Epub March 26, 2020. CrossRef PubMed
- Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med 2020;201:1372–9. CrossRef PubMed
- Gold JAW, Wong KK, Szablewski CM, et al. Characteristics and clinical outcomes of adult patients hospitalized with COVID-19—Georgia, March 2020. MMWR Morb Mortal Wkly Rep 2020;69:545–50. CrossRef PubMed
- CDC. National diabetes statistics report, 2020. Atlanta, GA: US Department of Health and Human Services, CDC; 2020. https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.Pdf
- Garg S, Kim L, Whitaker M, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019—COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:458–64. CrossRef PubMed
- US Census Bureau. Annual population estimates. Washington, DC: US Census Bureau; 2019. https://www.census.gov/newsroom/press-kits/2019/national-state-estimates.html
- Bureau of Labor Statistics. Labor force characteristics by race and ethnicity, 2018. Washington, DC: US Department of Labor, Bureau of Labor Statistics; 2019. https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htm
- Chowkwanyun M, Reed AL Jr. Racial health disparities and Covid-19—caution and context. N Engl J Med 2020. Epub May 6, 2020. CrossRef PubMed
Abbreviations: COVID-19 = coronavirus disease 2019; IQR = interquartile range.
* Includes data from laboratory-confirmed cases reported to CDC as of May 18, 2020.
† Data from laboratory-confirmed cases reported to CDC as of April 24, 2020, from these 16 public health jurisdictions: Alaska Department of Health and Social Services; Colorado Department of Public Health and Environment; Indiana State Department of Health; Louisiana Department of Health; Maine Center for Disease Control and Prevention; Michigan Department of Health and Human Services; Minnesota Department of Health; New Jersey Department of Health; New York City Department of Health and Mental Hygiene; North Carolina Department of Health and Human Services; Oregon Health Authority; Tennessee Department of Health; Utah Department of Health; Vermont Department of Health; Washington State Department of Health; Wisconsin Department of Health Services.
§ Persons who were not reported as Hispanic/Latino were all non-Hispanic.
¶ Includes persons reported as American Indian/Alaska Native (163 in case-based surveillance and 13 in supplementary data set), Native Hawaiian or other Pacific Islander (33 in case-based surveillance and eight in supplementary data set), multiracial, and persons of another race without further specification.
Abbreviations: COVID-19 = coronavirus disease 2019; ICU = Intensive care unit; IQR = Interquartile range; NH = non-Hispanic.
* Alaska Department of Health and Social Services; Colorado Department of Public Health and Environment; Indiana State Department of Health; Louisiana Department of Health; Maine Center for Disease Control and Prevention; Michigan Department of Health and Human Services; Minnesota Department of Health; New Jersey Department of Health; New York City Department of Health and Mental Hygiene; North Carolina Department of Health and Human Services; Oregon Health Authority; Tennessee Department of Health; Utah Department of Health; Vermont Department of Health; Washington State Department of Health; Wisconsin Department of Health Services.
† Includes persons reported as American Indian/Alaska Native (130), Native Hawaiian or other Pacific Islander (eight), multiracial, and persons reported as being of another race without further specification.
§ Includes decedents for whom at least one of the following conditions were reported: cardiovascular disease, diabetes mellitus, chronic kidney disease (including end-stage renal disease), neurologic conditions, immunosuppression, chronic liver conditions, or obesity. Conditions are not mutually exclusive; decedents might have more than one underlying condition.
¶ Includes decedents with hypertension, coronary artery disease, congenital heart disease, congestive heart failure, cerebrovascular accident/stroke, valvular heart diseases, conduction disorders, or other cardiovascular diseases.
** Includes only decedents for whom the condition within the specified category was collected from reviews of medical records.
†† Includes only decedents for whom data abstractors indicated did not have any condition within the specified category.
§§ Includes decedents for whom no data were available to indicate whether the decedent had any of the condition(s) within the specified category.
¶¶ Includes decedents with chronic kidney disease and end-stage renal disease.
*** Includes decedents with chronic obstructive pulmonary disease/emphysema, asthma, and tuberculosis.
††† Includes decedents with dementia, seizure disorders, and other neurologic conditions.
§§§ Includes decedents with any history of cancer, HIV/AIDS, or identified as being immunosuppressed.
¶¶¶ Includes decedents with cirrhosis, alcoholic hepatitis, chronic liver disease, end-stage liver disease, hepatitis B, hepatitis C, or non-alcoholic steatohepatitis.
**** Includes persons with body mass index ≥30 kg/m2.
†††† Among 3,021 (28.4%) persons for whom illness onset and death dates were reported; these data were available for 1,363 decedents aged <65 years, 557 decedents aged 65–74 years, 551 decedents aged 75–84 years, and 550 decedents aged ≥85 years.
§§§§ Includes decedents with a reported hospital admission date or who were reported to have died in a hospital.
¶¶¶¶ Among 7,794 (73.2%) persons with available data regarding time from admission to death; these data were available for 2,178 decedents aged <65 years, 1,909 decedents aged 65–74 years, 2,065 decedents aged 75–84 years, and 1,642 decedents aged ≥85 years.
***** Includes decedents who died in a long-term care facility, skilled nursing facility, assisted living facility, or nursing home.
††††† Cells with numbers <20 were suppressed.
§§§§§ Includes decedents for whom no data on location of death were reported and those for whom “other” was specified for death location without any more specific information.
 start highlightFIGURE. Decedent race/ethnicity,* by age group, reported to supplemental COVID-19 surveillance (N = 10,647) — 16 U.S. public health jurisdictions,† February 12–April 24, 2020end highlight
start highlightFIGURE. Decedent race/ethnicity,* by age group, reported to supplemental COVID-19 surveillance (N = 10,647) — 16 U.S. public health jurisdictions,† February 12–April 24, 2020end highlight
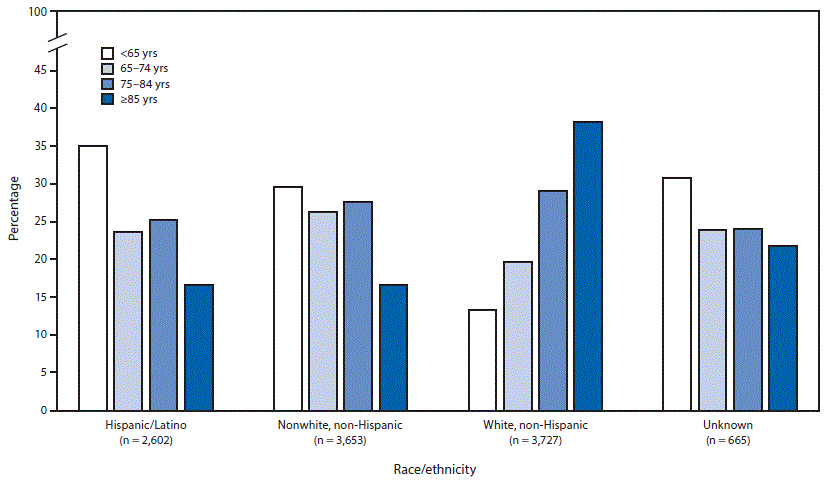
Abbreviation: COVID-19 = coronavirus disease 2019.
* start highlightThe “Nonwhite, non-Hispanic” group includes persons who are blackend highlight, Asian, American Indian/Alaska Native, or Native Hawaiian or other Pacific Islander; the “Unknown” group consists of persons for whom race/ethnicity data were not available.
† Alaska Department of Health and Social Services; Colorado Department of Public Health and Environment; Indiana State Department of Health; Louisiana Department of Health; Maine Center for Disease Control and Prevention; Michigan Department of Health and Human Services; Minnesota Department of Health; New Jersey Department of Health; New York City Department of Health and Mental Hygiene; North Carolina Department of Health and Human Services; Oregon Health Authority; Tennessee Department of Health; Utah Department of Health; Vermont Department of Health; Washington State Department of Health; Wisconsin Department of Health Services.
Suggested citation for this article: Wortham JM, Lee JT, Althomsons S, et al. Characteristics of Persons Who Died with COVID-19 — United States, February 12–May 18, 2020. MMWR Morb Mortal Wkly Rep 2020;69:923-929. DOI: http://dx.doi.org/10.15585/mmwr.mm6928e1.
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of
Health and Human Services.
References to non-CDC sites on the Internet are
provided as a service to MMWR readers and do not constitute or imply
endorsement of these organizations or their programs by CDC or the U.S.
Department of Health and Human Services. CDC is not responsible for the content
of pages found at these sites. URL addresses listed in MMWR were current as of
the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version (https://www.cdc.gov/mmwr) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Questions or messages regarding errors in formatting should be addressed to [email protected].