Immunity against cancer
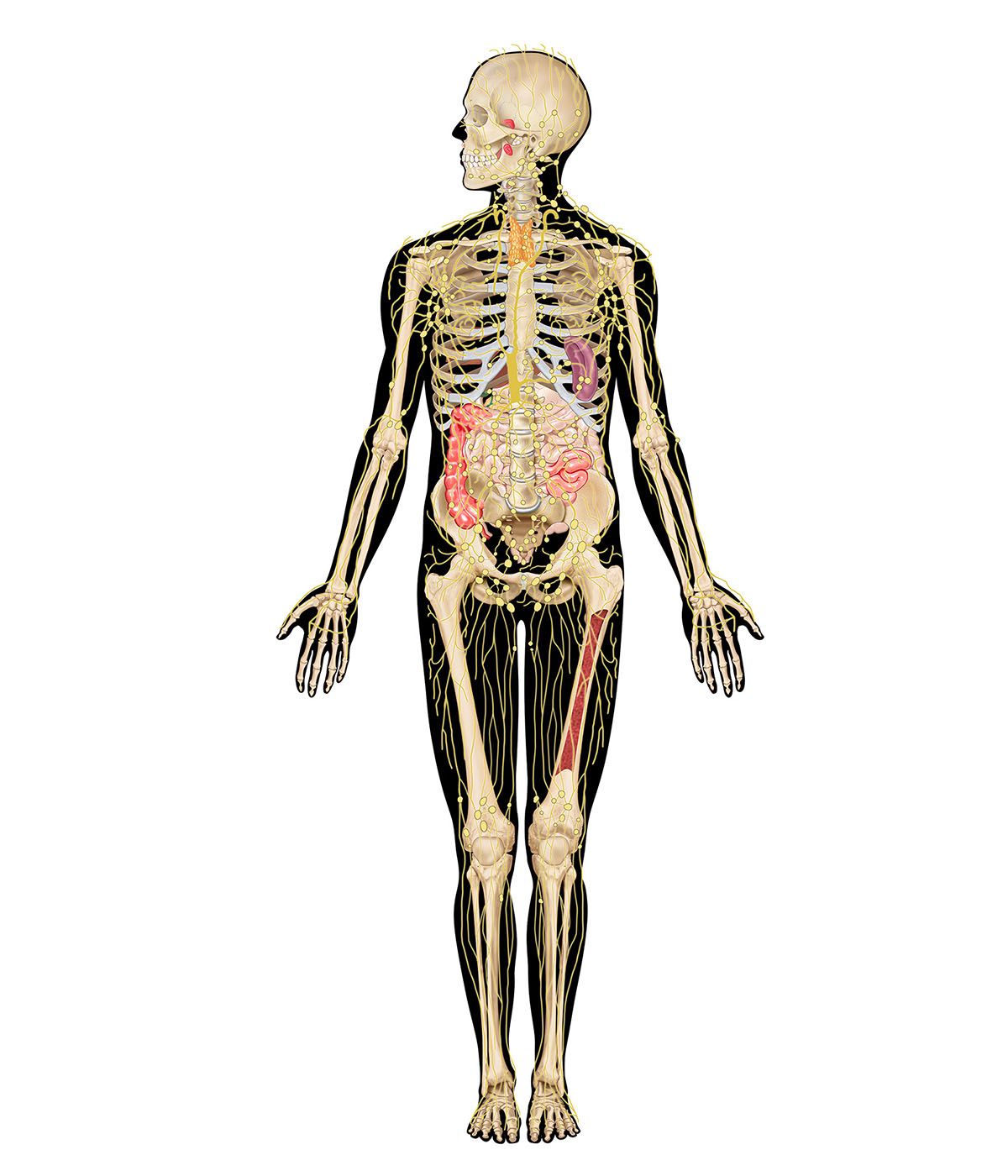
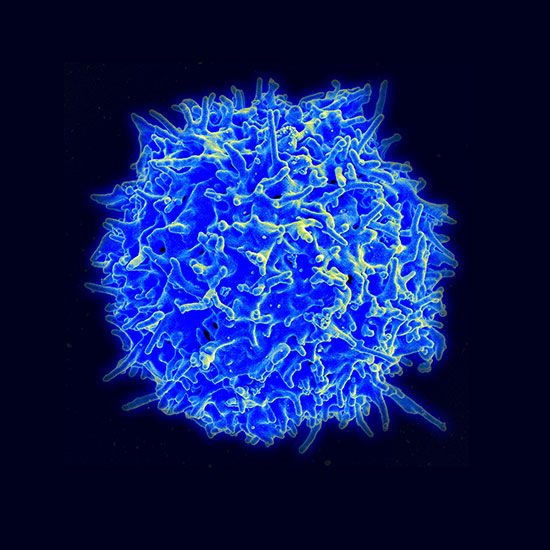
Cancer cells are normal body cells that have been altered in a manner that allows them to divide relentlessly, ignoring normal signals of restraint. As a result, cancer cells form clusters of cells, called tumours, that invade and colonize tissues, eventually undermining organ function and causing death. In the early 20th century the pioneering immunologist Paul Ehrlich pointed out that the enormous multiplication and differentiation of cells during prenatal life must afford many opportunities for aberrant cells to appear and grow but that immune mechanisms eliminate such cells. The idea that such a mechanism continues to function throughout life, weeding out newly arisen cancer cells, became popular in the 1950s and ’60s when a number of immunologists postulated immune surveillance, the theory that T-cell-mediated immunity evolved as a specific defense against cancer cells and that T cells constantly patrol the body, searching for abnormal body cells that carry antigens on their surface which are not found on healthy body cells. Although it has its compelling aspects, the immunosurveillance theory remains just a theory, and a controversial one at that.
The role of the immune system in protecting against cancer has not been fully explained, but nevertheless there is no question that in some instances the immune system can distinguish cancer cells from normal cells. The study of tumour immunology has shown unequivocally that cancer cells do carry antigens that are not present on healthy cells. Immunologists distinguish broadly between two types of tumour antigens: tumour-specific antigens, which are found only on cancer cells and not on their normal counterparts, and tumour-associated antigens, which are found on both normal and cancer cells but which are abnormally expressed—e.g., are overproduced—on cancer cells. In both cases these antigens have been shown to evoke an immune response, although not necessarily one strong enough to eliminate the tumour.
Why does a tumour continue to grow if an immune response against it is induced? Through animal experiments, a number of mechanisms have been identified that allow tumours to avoid recognition and destruction by the immune system:
- The surfaces of cancer cells may lose antigens that are recognizable by the immune system.
- Cancer cells may lose all class I MHC molecules from their surface, which prevents cytotoxic T cells from recognizing the cells.
- Some cancer cells produce immunosuppressive chemicals that can inhibit T cells directly or that can activate regulatory T cells.
- Some cancer cells shed some of their antigens, and these newly released, free-floating antigens may bind to the receptors on cytotoxic T cells, plugging them up so that the T cells cannot bind to the cancer cells and eliminate them.
- Certain cancer cells can outmaneuver an immune response by growing so rapidly or becoming such a dense mass that immune cells cannot come in contact with most of them.
Other dysfunctions of the immune system, such as immune suppression and immune deficiency, may contribute to cancer development and growth. Individuals such as transplant patients who have been treated with immunosuppressive drugs for a long period of time are more likely to develop certain types of cancer, as are patients with immunodeficiency diseases. For example, people with AIDS (acquired immunodeficiency syndrome) are more prone to developing cancers associated with viruses, such as Kaposi sarcoma. The incidence of cancer also increases greatly in old age, when some immune responses decline. But defective immune responses may not be the major factor involved in cancer development in the elderly, since genetic mutations that are linked to cancer also accumulate with age.
Much research has been devoted to developing effective immunotherapies against cancer. One avenue of research has focused on finding ways to immunize patients against the specific cancer growing within them. This approach targets tumour-specific antigens found on the cancer cells. Because these antigens are altered forms of normal self antigens, they are “foreign” and could be recognized by the immune system as such, but often they are not. However, investigators are working to develop vaccines that stimulate an immune response to these antigens, hoping that the reaction would be strong enough to eliminate the cancer.
Advances in scientists’ understanding of mechanisms underlying T-cell activation and immune regulation have facilitated the development of human monoclonal antibodies specifically tailored for the treatment of certain cancers. For example, the realization that a molecule known as CTLA-4 plays a role in downregulating immune responses against tumours led to the development of a therapeutic human monoclonal antibody against CTLA-4. Known as ipilimumab (Yervoy), the antibody was approved in 2011 by the U.S. Food and Drug Administration for the treatment of late-stage melanoma. Likewise, the discovery of a negative immune regulatory protein known as programmed cell death protein 1 (PD-1), which occurs on the surface of T cells, led to the development of highly effective anti-PD-1 cancer immunotherapies.
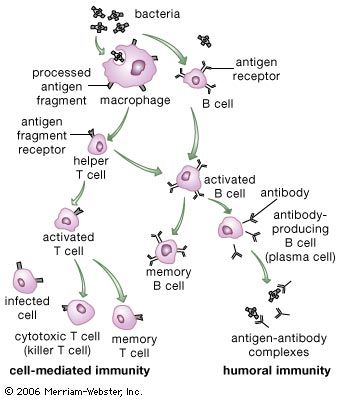
Prophylactic immunization
Prophylactic immunization refers to the artificial establishment of specific immunity, a technique that has significantly reduced suffering and death from a variety of infectious diseases. There are two types of prophylactic immunization: passive immunization, in which protection is conferred by introducing preformed antibodies or lymphocytes from another individual whose immune system was stimulated by the appropriate antigen, and active immunization, in which protection results from the administration of a vaccine, with dead or harmless living forms of an organism or with an inactivated toxin, that stimulates the immune system to produce lymphocytes and antibodies against that organism or toxin.
Passive immunization
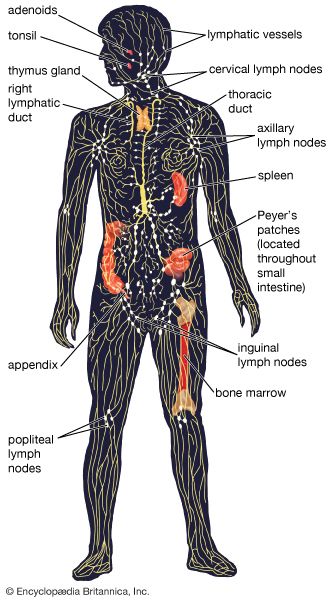
It is sometimes the case that an infectious organism or a poisonous substance can have such a rapid deleterious effect that the victim does not have time to develop an immune response spontaneously. At such times passive immunization with preformed antibodies can provide life-saving assistance in combating the pathogen or poison. This situation may arise in victims of poisonous snakebites or botulism, as well as in those in whom such infections as diphtheria, tetanus, or gas gangrene have progressed to the point at which bacterial toxins have been absorbed into the bloodstream. It is also the case with bites from a rabid animal, although active immunization is begun at the same time, since the spread of the rabies infection to the central nervous system is relatively slow. Physicians use passive immunization as temporary protection for persons traveling to countries where hepatitis B is prevalent. Passive immunization provides antibodies to persons who suffer from B-cell deficiencies and are therefore unable to make antibodies for themselves (see immune system disorder: Immune deficiencies). Also, as discussed earlier, passive immunizations of anti-Rh antibody can prevent erythroblastosis fetalis.
Protective immunoglobulins—primarily of the IgG class—can be prepared from the blood of humans or other species (e.g., horses or rabbits) that have already developed specific immunity against the relevant antigens. These preparations are known as antiserums. (This explains the original term for passive immunization, which is serum therapy.) Human IgG is slowly broken down in the recipient’s body, the concentration falling by about one-half every three weeks, so that effective amounts of antibody can be present for two or three months. Human antiserum is used whenever it is available, because IgG from other species is far more likely to provoke an immune response that will eliminate the antibody and may lead to serum sickness (see immune system disorder: Type III hypersensitivity).
Active immunization
Active immunization aims to ensure that a sufficient supply of antibodies or T and B cells that react against a potential infectious agent or toxin are present in the body before infection occurs or the toxin is encountered. Once it has been primed, the immune system either can prevent the pathogen from establishing itself or can rapidly mobilize the various protective mechanisms described above to abort the infection or toxin in its earliest stages.
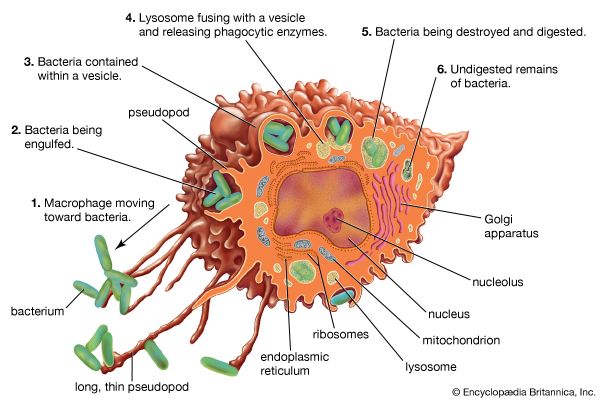
The vaccines used to provide active immunization need not contain living microbes. What matters is that they include the antigens important in evoking a protective response and that those antigens be administered in a harmless form sufficient in amount and persistence to produce an immune response similar to the natural infection. Bacterial toxins, such as those that cause tetanus or diphtheria, can be rendered harmless by treatment with formaldehyde without affecting their ability to act as immunogens. These modified toxins, or toxoids, usually are adsorbed onto an inorganic gel before being administered, an approach that increases the likelihood that the toxoid will be retained in a macrophage. Toxoids elicit effective, long-lasting immunity against bacterial toxins. When immunization against several antigenic determinants is desired or the important antigenic component is not known, it may be prudent to use the entire microbe, which has been killed in a manner that does not alter it significantly. Such so-called “killed” vaccines are used to immunize against typhoid, pertussis (whooping cough), plague, and influenza, for example. In other cases, researchers have developed attenuated (i.e., weakened) strains of bacteria or viruses. Attenuated vaccines cause an infection but do not produce the full array of signs and symptoms of the disease, because the infectious agent multiplies to only a limited extent in the body and never reverts to the virulent form. The use of such live microbes provides the most effective prophylaxis of all, since they truly imitate a mild form of the natural infection. Such are the vaccines for yellow fever, poliomyelitis (oral vaccine), measles, rubella, and tuberculosis. Although sufficiently attenuated as far as healthy persons are concerned, live vaccines may cause the full disease in persons who have an immune deficiency.
Most vaccines are administered by injection, but a few are given orally. Ultimately mucosal vaccines (those administered to mucosal surfaces such as those lining the gut, nasal passages, or the urogenital tract) may be the most effective vaccines available because of their unique ability to stimulate IgA responses and because of their ease of administration. Recombinant DNA technology has allowed researchers to use modified bacteria and viruses that are not harmful to humans to immunize individuals against an antigen from a pathogenic microorganism. This approach involves introducing into the DNA of the harmless microorganism a gene from a pathogenic organism that encodes an antigen capable of eliciting a protective immune response but not the full-blown disease. Once inoculated into the host, the microorganism generates the protective antigen of the pathogen and immunizes the host. An effective oral vaccine against cholera was developed based on this approach.
Sometimes different strains of a microorganism, each characterized by a different antigenic determinant, give rise to the same disease. In such cases neither natural infection nor prophylactic immunization with any one strain protects against infection by the others. For example, a variety of virus strains cause the common cold, but it is impractical to immunize against each strain. On the other hand, although there are more than 60 different strains of pneumococci that can cause bacterial pneumonia, some strains are much more common than others. Consequently a vaccine containing antigens from up to 14 of the most common strains is useful in protecting persons at special risk.
Active immunization is often the most effective and least costly method of protecting against an infectious disease. Vaccination campaigns against many diseases, such as diphtheria, polio, and measles, have been tremendously successful. In cases in which 95 percent or more of the population at risk is protected and humans are the only reservoir of infection, active immunization can lead to the worldwide eradication of the infectious agent, as has been achieved in the case of smallpox.